J Clin Periodontol:游离龈移植修复种植体周围角化龈不足
2020-05-31 网络 网络
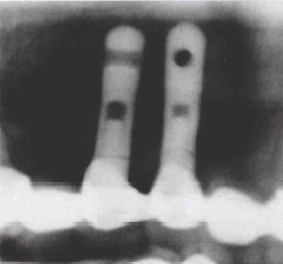
本研究是一项随机对照研究,旨在评估游离龈移植(FGGs)修复种植体周围角化龈(KM)<2mm后18个月的临床效果。
本研究是一项随机对照研究,旨在评估游离龈移植(FGGs)修复种植体周围角化龈(KM)<2mm后18个月的临床效果。
获取FGG组18个种植体(11个患者)和对照组8个种植体(7个患者)术后48个月的随访数据。对照组中的8个种植体在18个月后进行了FGGs,构成延迟FGG组(5个患者)。检测Km宽度、牙龈退缩(MR)和骨水平(CBL)。
结果发现,FGG组中Km宽度增加和MR降低保持了48个月,且MR值较非手术组低。在48个月内,非手术组的骨吸收(0.4±0.4mm)明显高于FGG组(0±0.4mm)。与FGG前相比,延迟FGG组MR降低,CBL没有显着差异。
因此,FGGs可能是一种修复种植体周围KM不足的实用方法。
原文出处:
Se‐LimOh, Free gingival grafts for implants exhibiting a lack of keratinized mucosa: Extended follow‐up of a randomized controlled trial,Journal of clinical periodontology, 2020 June,doi: 10.1111/jcpe.13272
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#种植#
40
#PE#
30
#种植体#
36
#角化龈#
49