JAMA:成人睡眠呼吸暂停患者气道正压通气与心血管事件和死亡的关系
2017-07-12 zhangfan MedSci原创
对于睡眠呼吸暂停患者,进行正压通气不能降低患者心血管事件发生率以及死亡风险。尽管正压通气有助于睡眠呼吸暂停症状的缓解,但其不能改变睡眠呼吸暂停患者心脏风险高的事实。
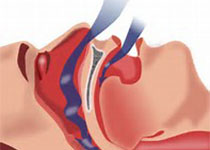
睡眠呼吸暂停(阻塞性和中枢性)与心血管危险因素相关,导致心血管疾病风险增加。无论是连续(CPAP)或自适应伺服 (ASV)正压通气(PAP)均可缓解睡眠呼吸暂停症状,但对于心血管风险的影响尚不清楚。近日研究人员考察了正压通气对于睡眠呼吸暂停引发的心血管风险的影响。研究人员对截止2017年3月的正压通气随机临床试验进行系统搜索,临床研究的主要研究内容心血管不良事件或死亡,考察相对风险(RR)和风险差异(RD)。主要终点是急性冠状动脉综合征(ACS)的复合事件,中风或血管性死亡(主要不良心血管事件);疾病特异性血管事件及死亡。研究包含了10项睡眠呼吸暂停正压通气临床研究(9 CPAP; 1 ASV),共7266名患者,平均年龄60.9岁,80.5%为男性,平均BMI 30.0。患者在期间发生了356起主要心血管不良事件以及613起死亡事件。正压通气不能降低主要心血管事件发生率 (RR, 0.77 [95% CI, 0.53-1.13]; P=0.19;RD, -0.01 [95% CI, -0.03-0.01]; P=0.23), 心血管死亡 (RR, 1.15 [95% CI, 0.88
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#血管事件#
33
#睡眠呼吸#
25
#正压通气#
23
#呼吸暂停#
32