European Radiology:ASL上的这一征象可以预测颈动脉内膜切除术后的脑组织高灌注!
2022-08-18 shaosai MedSci原创
动脉自旋标记(ASL)是一种非侵入性的MR技术,通过使用磁性标记的动脉血作为内源性示踪剂对脑灌注进行成像。
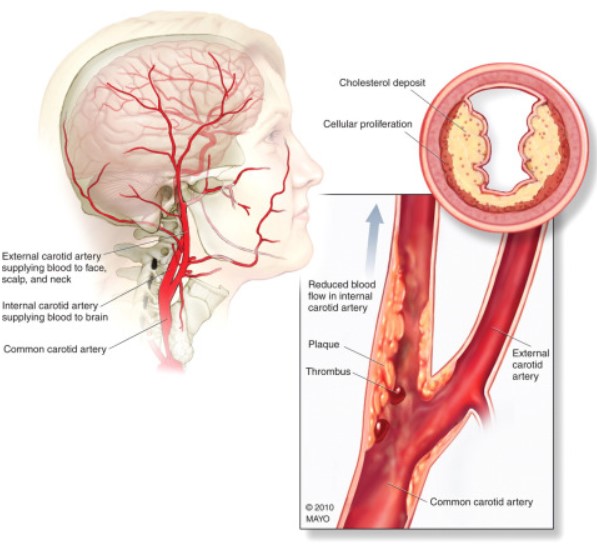
 作为颈动脉血管重建术后一种罕见但严重的并发症,脑过度灌注综合征(CHS)是术后出血性中风的重要原因之一。CHS常发生在脑过度灌注的病人身上,定义为与基线相比,灌注量增加100%以上。现阶段,最被广泛接受的脑灌注过度的机制是脑血管反应性(CVR)受损,不能通过血管收缩来维持稳定的脑血流(CBF)以应对血管重建后突然增加的脑灌注压力。使用乙酰唑胺或二氧化碳诱导的单光子发射计算机断层扫描(SPECT)在术前测量CVR是预测颈动脉内膜切除术(CEA)后脑部过度灌注的金标准。然而,考虑到乙酰唑胺或二氧化碳的潜在副作用,对所有患者进行CVR检查往往是不现实的。
作为颈动脉血管重建术后一种罕见但严重的并发症,脑过度灌注综合征(CHS)是术后出血性中风的重要原因之一。CHS常发生在脑过度灌注的病人身上,定义为与基线相比,灌注量增加100%以上。现阶段,最被广泛接受的脑灌注过度的机制是脑血管反应性(CVR)受损,不能通过血管收缩来维持稳定的脑血流(CBF)以应对血管重建后突然增加的脑灌注压力。使用乙酰唑胺或二氧化碳诱导的单光子发射计算机断层扫描(SPECT)在术前测量CVR是预测颈动脉内膜切除术(CEA)后脑部过度灌注的金标准。然而,考虑到乙酰唑胺或二氧化碳的潜在副作用,对所有患者进行CVR检查往往是不现实的。
动脉自旋标记(ASL)是一种非侵入性的MR技术,通过使用磁性标记的动脉血作为内源性示踪剂对脑灌注进行成像。在各种类型的脑血管疾病中,ASL可以提供与SPECT相当的CBF值。ASL的缺陷是对动脉到达时间的敏感性。如果动脉到达时间长于标记后的延迟时间,标记的血液就会在短时间内消失。标记延迟,标记的血液将在成像时留在血管中。在ASL图像上表现为明亮的绢状或斑点状的血管内信号,即所谓的动脉转运伪影(ATAs)。然而,这种 "伪影 "实际上可以成为一种有用的成像标记,因为它常常表明由于血管狭窄或侧支通路造成的血液延迟到达相应的血管区域。
基于ATAs的存在,Zaharchuk等学者开发了一个可靠的ASL评分用于评估侧支流量。在严重的颈动脉狭窄和侧支流不足的情况下,脑灌注压在狭窄的远端严重下降,甚至低于自动调节机制的补偿能力。术前不良的侧支条件增加了颈动脉再通后过度灌注的风险。
近日,发表在European Radiology杂志的一项研究评估了这种基于ATA的ASL评分预测颈动脉狭窄患者CEA后脑过度灌注的价值,为临床术前预测CEA后脑过度灌注提供了一个有价值的非侵入性方法。
本研究纳入了2015年5月至2021年7月期间接受CEA的连续颈动脉狭窄患者。对于每一位患者,通过将术后CBF与术前CBF图像除以两次伪连续ASL扫描获得脑血流比(rCBF)图。提取rCBF>2的高灌注区域,并对rCBF进行加权以计算高灌注指数。根据超灌注指数的分布,将患者分为超灌注组和非超灌注组。术前ASL图像根据10个感兴趣区域是否存在动脉转运伪影(ATAs)进行评分,对应于阿尔伯塔中风计划早期计算机断层成像评分方法。狭窄的程度以及主要和次要的侧支循环被评估为与ASL评分相关。进行了Logistic回归和ROC曲线分析以评估ASL评分对脑过度灌注的预测能力。
在纳入的86名患者中,有17名(19.8%)患者存在脑过度灌注。颈动脉近端闭塞、后交通动脉开放且前半环不完整以及脑外膜沟通与较低的ASL评分有关(P < 0.05)。术前ASL评分是脑过度灌注的独立预测因素(OR = 0.48 [95% CI [0.33-0.71]],p < 0.001),最佳截断值为25分(AUC = 0.98,94.1%敏感性,88.4%特异性)。
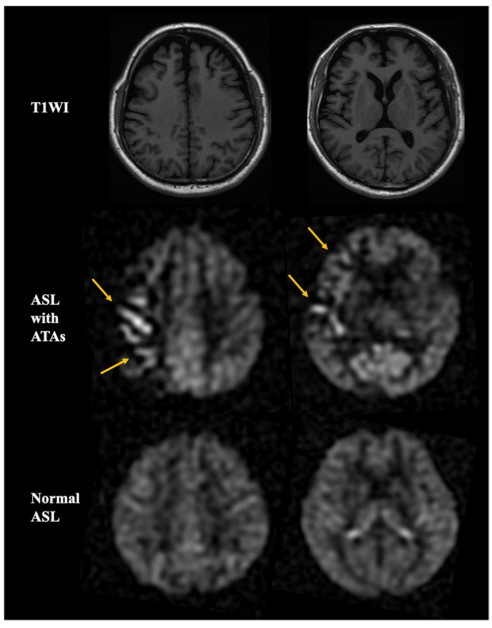
图 有动脉转运伪影(ATAs)的动脉自旋标记(ASL)和没有ATAs的正常ASL的代表性图像
本研究表明,ASL MRI出现的ATA是一个十分有临床价值的成像标记,可以通过目测获得且无需复杂的后处理步骤。基于ATA的存在,术前ASL可以预测颈动脉狭窄患者CEA后的脑部过度灌注。本研究结果支持将ASL技术应用于临床实践,对颈动脉狭窄术后并发症进行风险评估。
原文出处:
Xiaoyuan Fan,Zhentao Zuo,Tianye Lin,et al.Arterial transit artifacts on arterial spin labeling MRI can predict cerebral hyperperfusion after carotid endarterectomy: an initial study.DOI:10.1007/s00330-022-08755-x
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#切除术#
47
#高灌注#
58
#PE#
49
#内膜#
58
#颈动脉#
42
#ASL#
41
#脑组织#
47