Neurosurgery:颈动脉夹层患者可进行血管内治疗
2015-10-26 phylis 译 MedSci原创
背景:颈动脉夹层(CAD)的患者发生急性缺血性卒中(AIS)后血管内治疗的安全和可行性尚不清楚。目的:报道研究者CAD发生AIS患者进行干预措施,并通过系统性综述CAD的静脉溶栓(IVT)等传统治疗和CAD发生AIS的干预措施相比较。方法:回顾性分析来自两个第三中心的狭窄闭塞的CAD患者,患者NIHSS分数>5并且症状持续<12小时。搜索PubMed数据库系统综述CAD患者的进行IVT
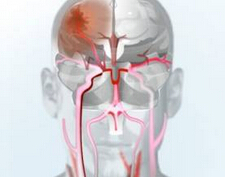
背景:颈动脉夹层(CAD)的患者发生急性缺血性卒中(AIS)后血管内治疗的安全和可行性尚不清楚。
目的:对CAD患者发生AIS进行干预措施后,并通过系统性综述,CAD的静脉溶栓(IVT)等传统治疗和CAD发生AIS的干预措施相比较。
方法:回顾性分析来自两个第三中心的狭窄闭塞的CAD患者,患者NIHSS分数>5并且症状持续<12小时。搜索PubMed数据库系统综述CAD患者的进行IVT治疗的研究。
结果:研究期间,进行血管内干预的患者1112名。21名患者满足纳入标准。患者平均年龄52.0 ± 10.9 岁,76% 为男性,NIHSS分数为17.4 ± 5.8; 52% 患者干预前进行IVT 并且90%患者存在串联闭塞。闭塞的平均时间为4.8 ± 2.1小时,处理时间为 1.8 ± 1.0小时。52%的患者应用支架,95%的患者获得再灌注。没有发生实质出血,71%的患者预后良好。8个涉及CAD患者溶栓的研究满足纳入标准(n=133)。与以前报道的IVT相比,研究者进行血管内治疗的患者,NIHSS分数较高(17 vs14),治疗前的时间较长(287 vs 162分钟)。与欧洲合作
急性卒中研究相比,患者症状性脑出血较少(0-6%),预后良好(71%-52%)。
结论:研究为CAD患者发生AIS进行血管内处理的可行性和安全性提供了证据。
原文出处:
Haussen DC, Jadhav A, Jovin T, et al. Endovascular Management vs Intravenous Thrombolysis for Acute Stroke Secondary to Carotid Artery Dissection: Local Experience and Systematic Review. Neurosurgery. 2015,Oct 21.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#颈动脉#
26
#颈动脉夹层#
36
#surgery#
30
#GER#
36
赞
135
#ROS#
31
#动脉夹层#
33
赶
117