European Radiology:当诊断为多发性原发性肺癌时,不同影像学征象预示着什么?
2022-04-08 shaosai MedSci原创
计算机断层扫描(CT)是定位病变和提供肺癌基本诊断信息的首选影像学手段。在治疗方面,最近的一些报道显示不同分子类型的sMPLC患者的肿瘤经过不同方法的治疗后,可获得较好的临床预后。
 多发性原发性肺癌(MPLC)是肺癌的一种特殊类型,于1975年由Martini和Melamed两位学者首次提出,并将其分为同步性多发性原发性肺癌(sMPLC)和非同步性多发性原发性肺癌(mMPLC。sMPLC是指在同一患者身上同时发生两个或两个以上的原发性肺癌,两个恶性肺肿瘤的诊断间隔时间在6个月以内。在过去的十年中,由于诊断方法和筛查程序的发展,sMPLC的检出率一直在增加。
多发性原发性肺癌(MPLC)是肺癌的一种特殊类型,于1975年由Martini和Melamed两位学者首次提出,并将其分为同步性多发性原发性肺癌(sMPLC)和非同步性多发性原发性肺癌(mMPLC。sMPLC是指在同一患者身上同时发生两个或两个以上的原发性肺癌,两个恶性肺肿瘤的诊断间隔时间在6个月以内。在过去的十年中,由于诊断方法和筛查程序的发展,sMPLC的检出率一直在增加。
计算机断层扫描(CT)是定位病变和提供肺癌基本诊断信息的首选影像学手段。在治疗方面,最近的一些报道显示不同分子类型的sMPLC患者的肿瘤经过不同方法的治疗后,可获得较好的临床预后。临床上,基因突变分析一般需要获取肿瘤组织样本。然而,有时从所有的肺部病变中获取足够的组织样本并不可行。一些研究者指出,将肺癌的CT特征与临床变量相结合,可用于预测表皮生长因子受体(EGFR)突变状态,但这些研究主要集中在单发性原发性肺癌。
近日,发表在European Radiology杂志的一项研究探讨了sMPLC的影像学分类、基因突变状态和手术预后之间的关系,为该类患者的进一步治疗及评估提供了有价值参考依据。
本研究从2013年1月到2019年10月期间对192名sMPLC患者进行了评估。对所有患者的临床、CT、分子和病理特征进行了分析。此外,还评估了89名只接受了手术切除的患者的预后情况。
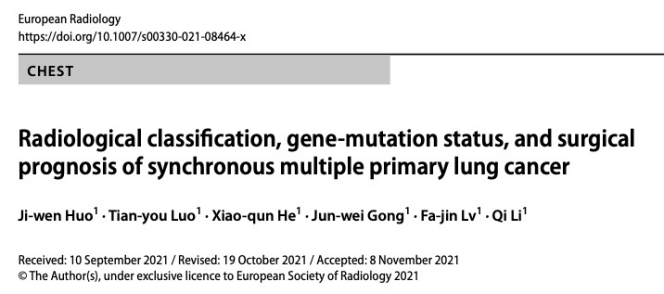
在192名患者中,对所有病理证实或根据影像学结果高度怀疑为肿瘤的病变进行了回顾性分析,并将sMPLC的CT结果分为三种类型。
(I)所有病变表现为实性结节/肿块(14.06%,27/192),
(II)所有病变表现为亚实性结节/肿块(43.23%,83/192),
(III)肿瘤病变表现为以下模式中2种及以上的组合:实性结节/肿块、亚实性结节/肿块、囊性空腔和局部实变(42.71%,82/192)。
对于252个接受表皮生长因子受体(EGFR)突变检测的肿瘤,表现为亚实性肿瘤的EGFR突变率高于实性肿瘤(P < 0.05)。在19名接受手术和基因检测的肿瘤患者中,基因异质性在多个病变中普遍存在(63.16%,12/19)。非I期的最高临床分期、同侧分布的肿瘤和I期的CT分类表明,sMPLC患者的预后较差(所有P<0.05)。
图 sMPLC的CT扫描分类。四位患者的肺窗的CT图像。A 患者1:CT分类I。一名68岁的男性(a,b),显示右肺上叶有一个KRAS突变的实性结节,左肺下叶有另一个野生型突变的实性肿块。B 患者2:CT分类为II级。一位65岁的女性(a,b),显示右肺上叶有一个19-del突变的亚实性结节,左肺上叶有另一个L858R突变的亚实性结节。C 患者3:CT分级为III级。一位71岁的男性(a,b),显示右肺下叶有一个EGFR突变的亚实性结节,左肺下叶有另一个野生型突变的实性肿块。D 患者4:CT分类为III级。54岁男性(a, b, c),显示右肺上叶有EGFR突变的囊性病变,右肺中叶有野生型突变的实性结节,左肺上叶有另一个EGFR突变的实性病变
总之,亚实性病变是sMPLC最常见的影像学表现,sMPLC之间可能存在驱动基因突变的遗传异质性。sMPLC患者的预后由多个肿瘤中的最高临床TNM分期、分布和影像学分类决定。非I期的最高临床分期、肿瘤同侧分布和I期的CT分类都表明sMPLC患者的预后较差。
原文出处:
Ji-Wen Huo,Tian-You Luo,Xiao-Qun He,et al.Radiological classification, gene-mutation status, and surgical prognosis of synchronous multiple primary lung cancer.DOI:10.1007/s00330-021-08464-x.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#原发性#
49
#多发性#
30
#PE#
33
感谢分享
46
#原发性肺癌#
34