欧盟批准Xeljanz(托法替尼)治疗溃疡性结肠炎
2018-08-01 MedSci MedSci原创
辉瑞公司近日宣布欧盟委员会扩大了Xeljanz(tofacitinib,托法替尼)的适应症,今后托法替尼能够治疗成人中度至重度活动性溃疡性结肠炎(UC),这些患者对传统疗法或生物制剂不耐受剂、反应不足或反应迟钝。
辉瑞公司近日宣布欧盟委员会扩大了Xeljanz(tofacitinib,托法替尼)的适应症,今后托法替尼能够治疗成人中度至重度活动性溃疡性结肠炎(UC),这些患者对传统疗法或生物制剂不耐受剂、反应不足或反应迟钝。该公司指出,该产品是第一种在该适应症中被批准的口服型JAK抑制剂。
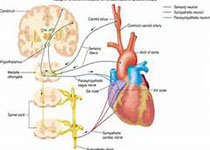
Xeljanz最初在欧盟被批准用于治疗对一种或多种改善疾病的抗风湿药物(DMARDs)反应不足或不耐受的成人中度至重度活动性类风湿性关节炎,以及甲氨喋呤不耐受或甲氨蝶呤治疗不适当的情况。早在2018年,该药物在欧洲被授权用于治疗既往接受DMARD治疗反应不足的成人活动性银屑病关节炎。托法替尼(tofacitinib)是辉瑞公司开发的一种JAK抑制剂,可有效抑制JAK1和JAK3的活性,阻断多种炎性细胞因子的信号转导。托法替尼相关的不良反应主要有头晕、头痛、胃肠道反应( 恶心、 腹泻) 、 鼻咽炎、 感染( 尤其是呼吸道和泌尿道感染) , 会导致中性粒细胞减少、 低密度和高密度脂蛋白以及胆固醇水平升高等,其中肠胃失调和感染最常见。
原始出处:
http://www.firstwordpharma.com/node/1582250#axzz5Mw2WiygQ
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#溃疡性#
22
类风湿和uc之间的发病机理是类似的吧
69
#欧盟批准#
31
#Xeljanz#
35
#治疗溃疡性结肠炎#
27
学习了,谢谢分享
68
学习了学习了,谢谢分享
68
学习了,谢谢
74
对于科研学习都有很大帮助
61
谢谢分享学习
22