BMJ:镰状细胞病血肿导致的眼眶梗死-案例报道
2017-02-16 xing.T MedSci原创
这个疾病可以与其他急性眼眶病变如眶蜂窝织炎混淆。这对患者视力构成了潜在的威胁,由于眼眶腔室综合征,并可与颅内血肿相关。
患者为5岁男孩,既往有镰状细胞病,因右眼框肿胀2天而就诊。该患者疑似眼眶蜂窝组织炎开始静脉注射抗生素治疗。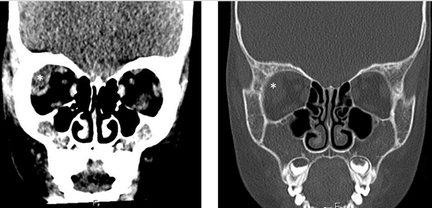
其体温正常,而且视力和眼球运动正常。计算机断层扫描(如图1所示)显示右上外侧有眼眶肿块,但没有鼻窦疾病。白细胞计数和C反应蛋白水平正常。最终诊断为眼眶外侧骨梗死,由于镰状红细胞,继发血肿。
这个疾病可以与其他急性眼眶病变如眶蜂窝织炎混淆。这对患者视力构成了潜在的威胁,由于眼眶腔室综合征,并可与颅内血肿相关。
原始出处:
Matthew R Edmunds, et al. Orbital infarction with haematoma in sickle cell disease.BMJ 2017; 356 doi: https://doi.org/10.1136/bmj.i6651
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#BMJ#
22
#眼眶梗死#
29
文意真好,值得分享
52
#血肿#
23
#眼眶#
31
#镰状细胞#
25
lixdch学习课堂
44