Cancer:去势耐受性前列腺癌患者肝和/或肺转移后接受enzalutamid治疗效果更好
2016-09-29 Fanfan 译 MedSci原创
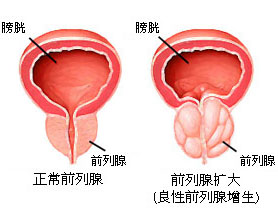
背景:去势耐受性(抵抗性)前列腺癌CRPC的定义:经过初次持续性内分泌治疗后疾病依然进展的前列腺癌,同时具备:(1)血清睾酮达到去势水平(小于50ng/dl或小于1.7nmol/L)(2)间隔一周,连续3次PSA上升,较最低值升高50%以上。可以这么认为,这样的患者一定是接受了内分泌治疗,可以是单纯的抗雄治疗,也可以是单纯的去雄治疗,也可以是联合应用,但一定是持续性内分泌治疗;疾病进展包括症状的出
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#耐受性前列腺癌#
36
#治疗效果#
28
文章很好,继续关注
61
#耐受性#
35
#肺转移#
37
谢谢分享,学习了
61