Blood:Selinexor联合低剂量硼替佐米和地塞米松(SVd)用于复发性/难治性多发性骨髓瘤的疗效和安全性
2018-10-26 MedSci MedSci原创
中心点:Selinexor联合低剂量的硼替佐米和地塞米松(SVd)用于复发性/难治性多发性骨髓瘤患者,安全且耐受性好。SVd疗法可获得较高的缓解率,PI非难治性患者ORR可达84%,而PI复发性患者的ORR也可达到43%。摘要:Selinexor是一种口服的核输出蛋白exportin1(XPO1)抑制剂。预临床研究表明,selinexor和蛋白酶体抑制剂(PI)可通过抑制NFκB信号和肿瘤抑制蛋白
Selinexor联合低剂量的硼替佐米和地塞米松(SVd)用于复发性/难治性多发性骨髓瘤患者,安全且耐受性好。
SVd疗法可获得较高的缓解率,PI非难治性患者ORR可达84%,而PI复发性患者的ORR也可达到43%。
摘要:
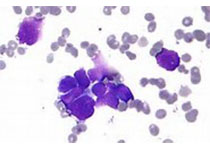
Selinexor是一种口服的核输出蛋白exportin1(XPO1)抑制剂。预临床研究表明,selinexor和蛋白酶体抑制剂(PI)可通过抑制NFκB信号和肿瘤抑制蛋白的核保留协同发挥抗骨髓瘤活性。
Nizar J. Bahlis等人对selinexor联合低剂量的硼替佐米和地塞米松(SVd)用于复发性/难治性多发性骨髓瘤(MM)患者的疗效和安全性进行评估。主要结点是明确SVd联合方案的安全性、总体缓解率(ORR)和适宜用于II期研究的剂量(RP2D)。研究人员共招募了42位复发性/难治性多发性骨髓瘤患者,予以selinexor(60、80或100mg 口服)、硼替佐米(1.3mg/m2 皮下注射)和地塞米松(20mg 口服),1次/周或2次/周,21天或35天一疗程。患者既往治疗中位次数为3次(1-11),50%的患者PI难治性。
常见的治疗相关的3/4级副反应(发生在10%以上的患者中的)有血小板减少(45%)、中性粒细胞减少(24%)、疲惫(14%)和贫血(12%)。周围神经病变的发生率(4位[10%])和等级(≤2)均较低。患者总体缓解率(ORR)为63%,PI非难治性患者高达84%,而PI难治性患者也可达43%。所有患者的中位无进展存活期为9.0个月;PI非难治性和PI难治性患者的分别是17.8个月和6.1个月。
综上所述,对于复发性/难治性多发性骨髓瘤患者,包括硼替佐米难治性患者,SVd疗法缓解率高,且无意料之外的副作用。推荐的II期试验剂量:selinexor(100mg 1/周)、硼替佐米(1.3mg/m2 1/周,连用4周)和地塞米松(40mg 1/周),35天一疗程。
Nizar J. Bahlis,et al. Selinexor plus low-dose bortezomib and dexamethasone for patients with relapsed or refractory multiple myeloma. Blood 2018 :blood-2018-06-858852; doi: https://doi.org/10.1182/blood-2018-06-858852
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#多发性#
27
#疗效和安全性#
33
#复发性#
27
#复发性/难治性多发性骨髓瘤#
43
#低剂量#
28
#难治性#
24
#selinexor#
33
谢谢梅斯提供这么好的信息,学到很多
41