Blood:二代测序证实最小残余病灶可作为多发性骨髓瘤的预后标志物
2018-09-25 MedSci MedSci原创
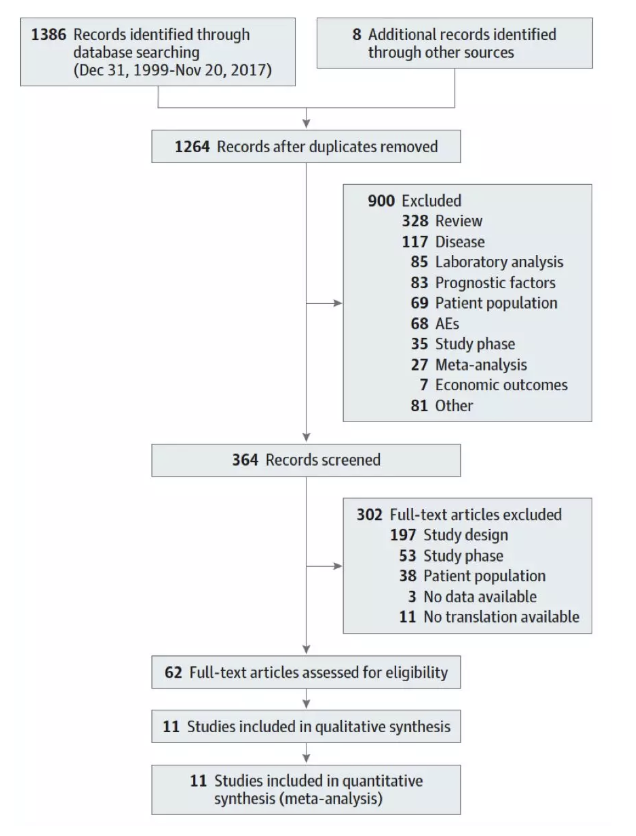
新型药物的引入极大程度的提高了多发性骨髓瘤患者的临床预后。为缩短新疗法的评估时间,卫生机构目前正在尝试以最小残留病灶(MRD)作为临床试验的替代评估结点。Aurore Perrot等人在维持治疗阶段采用二代测序来评估MRD的预后意义。MRD阴性定义:在1000000个骨髓细胞内无肿瘤浆细胞(<10-6)。数据分析来源于近期一个评估移植在对于新确诊的采用来那度胺、硼替佐米和地塞米松(RVD)治
Aurore Perrot等人在维持治疗阶段采用二代测序来评估MRD的预后意义。MRD阴性定义:在1000000个骨髓细胞内无肿瘤浆细胞(<10-6)。数据分析来源于近期一个评估移植在对于新确诊的采用来那度胺、硼替佐米和地塞米松(RVD)治疗的骨髓瘤患者的意义的临床试验。
本研究通过二代测序证明了MRD状态可作为多发性骨髓瘤的预后生物标志物,提示该方法或可用于适应未来临床试验的治疗策略。
Aurore Perrot,et al.Minimal residual disease negativity using deep sequencing is a major prognostic factor in multiple myeloma. Blood 2018 :blood-2018-06-858613; doi: https://doi.org/10.1182/blood-2018-06-858613
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#预后标志#
36
#多发性#
31
#标志物#
27
#二代测序#
34
#预后标志物#
28
二代测序证实最小残余病灶。
72
学习了
66