Front Cardiovasc Med:HAS-BLED评分对AF患者出血风险的预测分析
2021-12-12 汪文慧 “心关注”公众号
心房颤动(AF)是临床实践中最常见的心律失常,与缺血性卒中的5倍风险相关。口服抗凝剂(OAC)可降低AF患者发生血栓栓塞的风险;然而,也增加出血风险。
心房颤动(AF)是临床实践中最常见的心律失常,与缺血性卒中的5倍风险相关。口服抗凝剂(OAC)可降低AF患者发生血栓栓塞的风险;然而,也增加出血风险,尤其是大出血和颅内出血,且与心血管不良事件发生率及死亡率的增加相关。因此,应对启用OAC治疗后的出血风险进行评估。2010年欧洲心脏调查数据库建立的HAS-BLED评分系统已被推荐为AF患者抗凝相关出血风险的常规预测。
除HAS-BLED评分外,针对AF患者还开发了其他几种出血风险评估模型。然而,HAS-BLED评分与其他风险评分的预测能力差异仍不确定。Chang G等人对18项涉及321,888例患者的研究进行了荟萃分析,发现在特异性和敏感性方面,HAS-BLED评分是最均衡的出血风险预测工具。然而,当考虑AF患者出血事件的可能性时,其对临床医生的指导有限。Zhu W等人进行的一项荟萃分析显示,与其他风险评分相比,HAS-BLED评分在预测大出血方面表现更好。然而,该研究只评估了使用维生素K拮抗剂的(VKA)AF患者的HAS-BLED评分;由于直接口服抗凝剂(DOACs)被推荐用于非瓣膜性AF患者卒中预防的首选药物,因此,HAS-BLED评分是否适用于DOAC治疗的患者尚不清楚。
为明确这一疑问,研究人员通过系统回顾的方法,评估在使用VKA或DOACs的AF患者中,HAS-BLED评分的准确性以及与其他风险评分相比,在预测出血方面的优劣。
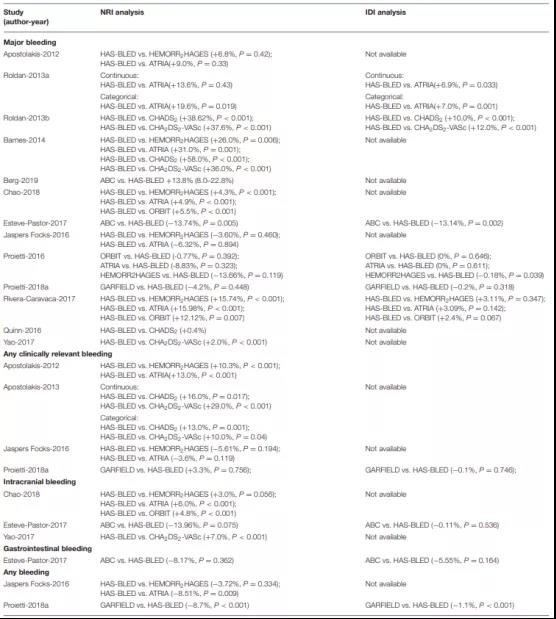
研究结果显示:在抗凝患者中,HAS-BLED评分预测大出血的C统计量为0.63(95%CI 0.61-0.65)(图1);VKA[0.63(0.59-0.67)],DOAC[0.63(0.61-0.65)](图2)。HAS-BLED 评分与HEMORR2HAGES评分、ATRIA评分、GARFIELD-AF评分和ABC评分的C 统计量相似;但显着高于CHADS2评分及CHA2DS2-VASc评分(表1)。NRI和IDI分析表明,HAS-BLED 评分优于CHADS2或CHA2DS2-VASc评分;与HEMORR2HAGES、ATRIA、ORBIT或GARFIELD-AF评分相比,具有相似或更好的预测能力(表2)。但由于证据有限,HAS-BLED评分与其他评分相比的校准和决策曲线分析需要进一步评估。
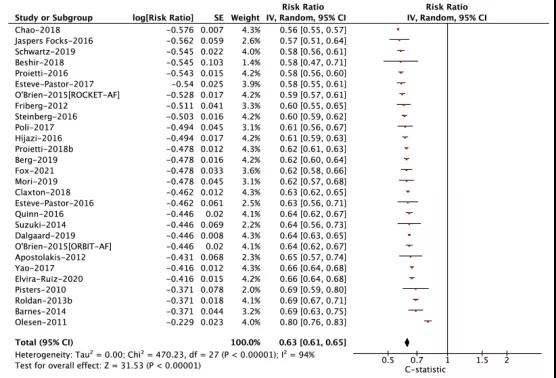
图1. AF抗凝患者大出血C统计量的汇总分析
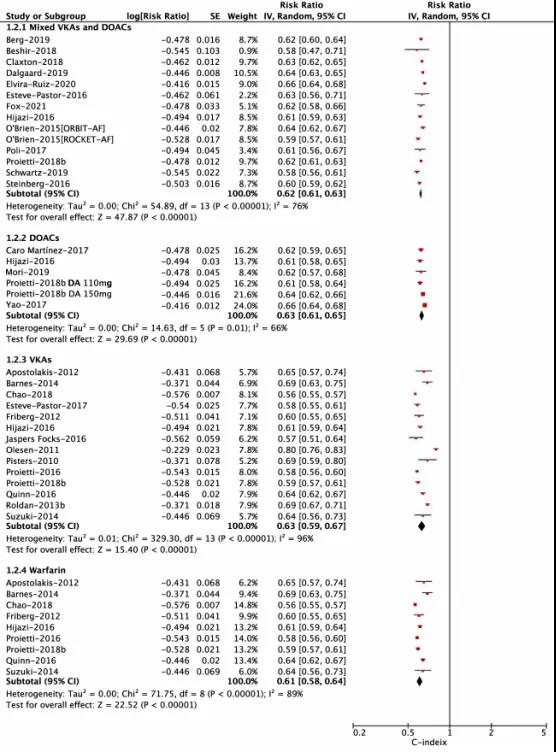
图2. 基于口服抗凝剂类型的HAS-BLED评分
表1. 纳入研究的C统计量和95%CI汇总
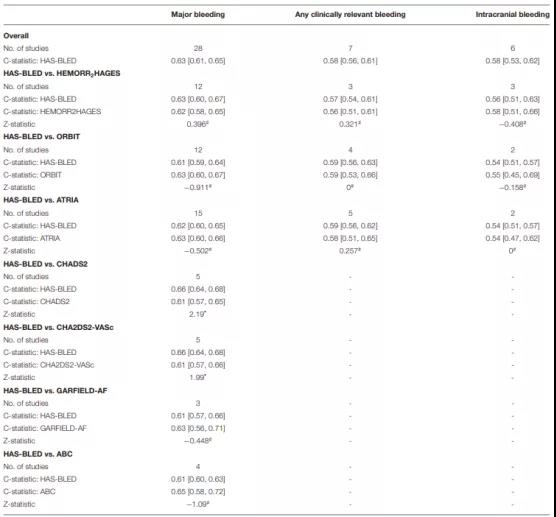
表2. 预测AF抗凝患者出血风险的NRI和IDI分析
以上结果表明无论使用何种口服抗凝剂,HAS-BLED 评分对AF患者的出血风险均具有中等预测能力。目前的证据支持HAS-BLED评分至少不劣于HEMORR2HAGES、ATRIA、ORBIT、GARFIELD-AF、CHADS2、CHA2DS2-VASc或ABC评分。
原始出处:
Xinxing Gao, et al. Diagnostic Accuracy of the HAS-BLED Bleeding Score in VKA- or DOAC-Treated Patients With Atrial Fibrillation: A Systematic Review and Meta-Analysis. Front. Cardiovasc. Med., 22 November 2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#LED#
48
#ASC#
34
#AF患者#
32
#Med#
42