Hypertension:血压波动大,老人认知功能减退加快!
2016-05-24 MedSci MedSci原创
人的血液输送到全身各部位需要一定的压力,这个压力就是血压。常规采用收缩压和舒张压等数据表示机体血压。单位为毫米汞柱(mmHg)。心室收缩,血液从心室流入动脉,此时血液对动脉的压力最高,称为收缩压(SBP )。心室舒张,动脉血管弹性回缩,血液仍慢慢继续向前流动,但血压下降,此时的压力称为舒张压(DBP)。理想血压是收缩压< 120 mmHg、舒张压<80mmHg。正常血压是90mmHg&
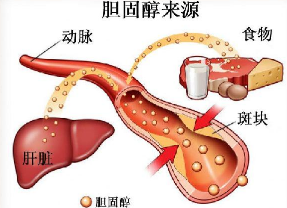
人的血液输送到全身各部位需要一定的压力,这个压力就是血压。常规采用收缩压和舒张压等数据表示机体血压。单位为毫米汞柱(mmHg)。心室收缩,血液从心室流入动脉,此时血液对动脉的压力最高,称为收缩压(SBP )。心室舒张,动脉血管弹性回缩,血液仍慢慢继续向前流动,但血压下降,此时的压力称为舒张压(DBP)。理想血压是收缩压< 120 mmHg、舒张压<80mmHg。正常血压是90mmHg<收缩压 <140mmHg、 60mmHg<舒张压<90mmHg。高血压是指动脉血压超过正常值的异常升高,通常为收缩压≥140mmHg或舒张压≥90mmHg,高血压民众患心脏病、卒中和心梗等心血管疾病的风险增加。
但越来越多的研究表明,血压随时间的波动也可能为民众带来健康风险,去年发表的一项研究表明,血压变异性可能增加民众患心血管疾病和死亡的风险。新布伦瑞克罗格斯大学癌症研究所的Bo Qin博士指出,老年人的血压波动可能会加速认知功能下降程度。
他们对976名年龄超过55岁的中国健康营养调查中的参与者进行了调查,并收集他们5年来的血压变异性和因血压问题就诊的相关数据。
参与者的血压变异性是评估5年来,通过血压测量在三个或四个医生的访问。此外,在5年内研究人员对每位参与者进行了大量的测试以评估参与者的认知功能。这些测试包括单词记忆和向后计数。
研究人员发现,5年内收缩压变化较大的参与者认知功能下降的程度更快,包括语言记忆和单词记忆能力。舒张压变化较大会使55-64岁的成年人认知功能减退较快,但是65岁以上的老人未出现这一特点。
尽管研究人员表示他们的研究并没有证明因果血压变异性和认知能力下降之间存在因果关系,但这表明血压变化较大增加民众的健康风险,因此他们建议医务人员密切关注中老人年人的血压变化。
研究人员认为,血压变异性可能是血流信号不稳定的暗示或信号,并导致大脑毛细血管的损伤,进而导致大脑结构和功能的变化。保持血压的稳定性有助于保护老年人的认知功能。研究人员表示仍需进行更进一步的研究。
原始出处:
Cognitive decline hastened with greater fluctuations in blood pressure,MNT,24,May,2016
Visit-to-visit variability in blood pressure is related to late-life cognitive decline, Bo Qin et al.Hypertension, 23 May 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PE#
38
#血压波动#
35
#TENS#
38
继续学习
46
继续关注
57
#Hypertension#
27