N Engl J Med:缓解干眼症 鱼油遭打脸
2018-06-24 MedSci 环球医学网
干眼症是临床上较常见的一种眼部疾病,患者会出现各种眼部不适症状,严重时甚至影响视觉功能。发表在《N Engl J Med》的一项多中心、双盲临床研究调查了n?3脂肪酸补充剂(通常叫做ω-3脂肪酸)治疗干眼症的疗效。
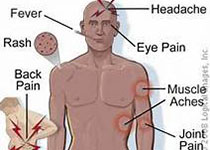
背景:干眼症是一种常见的慢性病,以眼部不适和视觉受阻为特征,进而降低生活质量。许多临床医师推荐使用n?3脂肪酸补充剂来缓解症状。
方法:在一项多中心、双盲临床研究中,研究者将中至重度干眼症患者随机分配至每天口服3000 mg鱼类n?3二十碳五烯酸和二十二碳六烯酸(积极补充组)或橄榄油安慰剂(安慰剂组)。主要结局指标为基于6个月和12个月评分平均值,眼表疾病指数(OSDI;评分范围0~100,评分越高显示症状严重程度越大)与基线相比的平均变化。次要结局指标包括每只眼睛结膜染色评分(范围:0~6)和角膜染色评分(范围:0~15)的平均变化,评分越高说明眼表损害越严重,以及泪膜破裂时间(眨眼的秒数和泪液膜裂痕)的平均变化,以及Schirmer测试的结果(下眼睑上放置的纸带的润湿长度),数值越低说明病情越严重。
结果:共有349例患者被分配至积极补充组,186例患者分配至安慰剂组;主要分析分别包括329例和170例患者。积极补充组与安慰剂组的OSDI评分平均变化没有显着差异(分别为?13.9分和?12.5分;在填补缺失的数据后变化的平均差异,?1.9分;95%置信区间[CI],?5.0~1.1;P=0.21)。预定亚组之间的结果具有一致性。积极补充组与安慰剂组在结膜染色评分(变化的平均差异,0.0分;95% CI,?0.2~0.1)、角膜染色评分(0.1分;95% CI,?0.2~0.4)、泪膜破裂时间(0.2秒;95% CI,?0.1~0.5)和Schirmer测试的结果(0.0 mm;95% CI,?0.8~0.9)方面与基线相比的平均变化没有显着差异。根据红细胞中n?3脂肪酸的水平,12个月时,积极补充组的依从率为85.2%。两组之间的不良事件率相似。
结果:在干眼症患者中,被随机分配至使用富含3000 mg n?3脂肪酸补充剂为期12个月的患者,其结局并不显着优于分配至使用安慰剂的患者。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Eng#
35
#Engl#
37
#干眼症#
33
#干眼#
37
#Med#
26
谢谢分享.学习了
67
谢谢分享.学习了
67