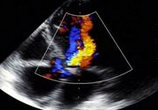
Sci Rep:结缔组织病患者的左心室变形
2019-12-18 xiangting MedSci原创
这项研究表明,尽管保留了LVEF,CTD患者仍表现出异常的LV变形。IIM与非IIM患者的LV变形损害有所不同。
这项研究目的是评估结缔组织病患者(CTD)的左心室(LV)心肌劳损,并比较特发性炎症性肌病(IIM)与非IIM亚组的LV变形。
入选了98名CTD患者,其中包括56名IIM患者和42名非IIM患者,以及30名健康受试者,并进行3.0T心脏磁共振成像(MRI)扫描。测量和评估了左室功能和应变参数。
研究结果表明,CTD患者左心室射血分数保留(60.85%),并且径向、周向和纵向的总体和区域峰值应变(PS)明显降低(p均<0.05)。IIM患者的总体纵向PS(GLPS)和心尖部纵向PS明显降低,而非IIM患者的所有应变参数均下降。除了GLPS和心尖部纵向PS外,非IIM患者的所有应变参数均低于IIM患者。通过Pearson相关性分析,IIM和非IIM患者的LV总体径向和周向PS均与N-末端前脑利钠肽水平和LV射血分数相关。
这项研究表明,尽管保留了LVEF,CTD患者仍表现出异常的LV变形。IIM与非IIM患者的LV变形损害有所不同。
原始出处:
Jin
Wang. Left Ventricular Deformation in Patients with Connective Tissue Disease:
Evaluated by 3.0T Cardiac Magnetic Resonance Tissue Tracking. Sci Rep. 29
November 2019.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心室变形#
26
#结缔组织#
38
了解一下
83
#结缔组织病#
43
#左心室#
40