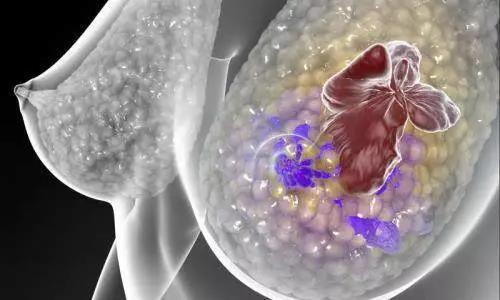
Sci Transl Med: 这些被忽视的免疫细胞,竟是乳腺癌细胞治疗的“潜力股”!
2019-10-25 Ruthy 转化医学网
乳腺癌是女性最常见的恶性肿瘤之一,也是当前社会的重大公共卫生问题。其中雌激素受体(ER)、孕激素受体(PR)和原癌基因Her-2均为阴性的三阴性乳腺癌(TNBC)恶性程度极高、预后极差,一旦转移多只能束手无策,因此,确定更为有效的乳腺癌治疗靶点成为了重中之重。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TRA#
30
#Transl#
32
#癌细胞#
23
#Med#
29
谢谢了,学习
63