NEJM:依度沙班治疗癌症相关的静脉血栓栓塞症疗效分析!
2017-12-13 xing.T MedSci原创
由此可见,对于复发性静脉血栓栓塞或大出血的复合结局,口服依达沙班并不劣于皮下注射达肝素钠。依达沙班组静脉血栓栓塞复发率较低,但大出血发生率高于达肝素钠组。
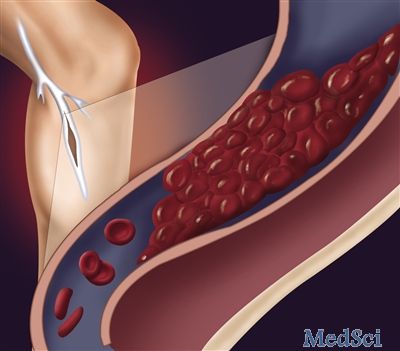
低分子量肝素是癌症相关性静脉血栓栓塞的标准治疗方法。然而,直接口服抗凝剂治疗的作用尚不清楚,近日,顶级医学期刊NEJM上针对这一问题发表了一篇研究文章。
在这项开放分组的非劣效性试验中,研究人员将具有急性症状或偶发静脉血栓栓塞的癌症患者随机分配接受低分子量肝素治疗至少5天,然后口服60mg依度沙班,每日一次(依度沙班组)或皮下注射达肝素钠,剂量为每公斤体重200IU,每日一次,持续1个月,接着以每天150IU/kg的剂量注射达肝素钠(达肝素钠组)。治疗至少6个月至12个月。该研究的主要终点是随机分组后12个月内复发性静脉血栓栓塞或大出血的复合终点,无论治疗持续时间。
在1050例接受随机分组的患者中,1046例患者被纳入改良的意向性治疗分析。依度沙班组552名患者中67例发生主要终点事件(12.8%),而达肝素钠组的524例患者中有71例(13.5%)(风险比为0.97,95%可信区间[CI]为0.70-1.36;非劣效性P=0.006;优势P=0.87)。依度沙班组有41例(7.9%)和达肝素钠组有59例(11.3%)患者发生静脉血栓栓塞(风险差异为-3.4%;95%CI为-7.0至0.2)。依度沙班组有36例(6.9%)和达肝素钠组有21例(4.0%)患者发生大出血(风险差异为2.9个百分点,95%CI为0.1-5.6)。
由此可见,对于复发性静脉血栓栓塞或大出血的复合结局,口服依度沙班并不劣于皮下注射达肝素钠。依度沙班组静脉血栓栓塞复发率较低,但大出血发生率高于达肝素钠组。
原始出处:
Gary E. Raskob,et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism.N Engl J Med 2018; 378:615-624 DOI: 10.1056/NEJMoa1711948
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#静脉血#
24
#静脉#
33
#癌症相关#
36
#癌症相关的静脉血栓栓塞#
25
#栓塞症#
34
#疗效分析#
22
了解了解.学习学习
74
学习
58
学习一下
60