Gastroenterology:沃诺拉赞(Vonoprazan)的使用综述
2020-02-03 不详 网络
沃诺拉赞(Vonoprazan,TAK-438)是一种钾离子竞争性酸阻滞剂又称为P-CAB,通过竞争性阻断H-K-ATP酶中钾离子的活性,来抑制酸分泌。它是目前由武田制药公司研发的吡咯衍生物,化学成分为1-[5-(2-氟苯基)-1-(吡啶-3-酰基磺酰)-1H-吡咯-3-酰基]-N-甲基甲醇胺富马酸盐。沃诺拉赞具有酸稳定性,空腹时可被快速吸收,进食后1.5至2小时达到Cmax。它解离缓慢(半衰
沃诺拉赞(Vonoprazan,TAK-438)是一种钾离子竞争性酸阻滞剂又称为P-CAB,通过竞争性阻断H-K-ATP酶中钾离子的活性,来抑制酸分泌。它是目前由武田制药公司研发的吡咯衍生物,化学成分为1-[5-(2-氟苯基)-1-(吡啶-3-酰基磺酰)-1H-吡咯-3-酰基]-N-甲基甲醇胺富马酸盐。沃诺拉赞具有酸稳定性,空腹时可被快速吸收,进食后1.5至2小时达到Cmax。它解离缓慢(半衰期约为7.7小时)。其高pKa值(>9)促进了它在壁细胞小管腔中的积聚,从而竞争性地抑制质子泵的开放和关闭。个体间有效性的差异与剂量,性别,年龄和CYP2C19有关。对于肾脏或肝脏疾病患者,不建议调整剂量。沃诺拉赞抑制CYP2B6和CYP3A4/5,它们延长了共同给药药物如克拉霉素的代谢。
沃诺拉赞克服了传统PPI疗法的许多弱点(即半衰期短,在酸性环境中的易被破坏,需要酸保护,仅抑制活化的质子泵,在达到完全效果之前需要3到5个周期的给药,以及与CYP2C19多态性相关的临床变异性)。沃诺拉赞已被日本批准用于治疗胃和十二指肠溃疡,治疗反流性食管炎和预防复发,二次预防小剂量阿司匹林或非甾体类抗炎药(NSAID)诱导的胃粘膜损伤,以及用于一线和二线幽门螺杆菌根除治疗。
▌沃诺拉赞与传统质子泵抑制剂(PPIs)的比较
沃诺拉赞比传统PPIs更有效且长效。临床上其他抗分泌药物的相对效力基于它们将胃内pH维持在期望值以上的能力。例如,对于溃疡愈合,pH>3;对于反流性食管炎,pH>4;对于幽门螺杆菌感染的治愈和预防内镜止血后再出血,pH>6。PPI的相对效力主要基于pH4时间,即经过5天以上的治疗后,24小时内胃内pH保持>4的时间。在奥美拉唑当量(OE)中定义的相对PPI效力,基于在西方群体中确定的pH4时间,其使用方式为每天一次和每天两次。相对而言,沃诺拉赞半衰期较长,因而被认为是最佳的b.i.d类PPI。
每天一次给予沃诺拉赞20mg,1天后达到约63%pH4时间,7天后增加至约84%。在西方人口的研究中,连续使用7天后,10,20,30,40mg的沃诺拉赞pH4时间的加权中位数分别为60.2%,85.2%,90.1%,93.2%。将这些结果外推至PPI的pH4时间表明,每天一次10mg的沃诺拉赞大约相当于60mg奥美拉唑,20mg大约相当于奥美拉唑60mg b.i.d.,也相当于埃索美拉唑40mg b.i.d.。这些相对效力可以评估沃诺拉赞和PPIs是否使用可比的抗分泌剂量有关的比较试验。但需要注意的是,大多数沃诺拉赞研究仅在日本人群中报道,目前关于PPI相对效力的数据仅在西方人群中确定。在这里,我们根据西方数据将沃诺拉赞与PPIs在亚洲人群中进行比较,PPIs通常更有效但更易变化,因为亚洲人群的CYP2C19多态性更大且壁细胞数量较低。总体而言,大多数PPI-沃诺拉赞的比较研究显示,使用沃诺拉赞的抗分泌剂量明显高于PPIs(60mg奥美拉唑,每日一次或两次)(10mg雷贝拉唑,OE=18mg; 20 mg埃索美拉唑,OE=32mg,30 mg兰索拉唑,OE=27mg,或15mg兰索拉唑,OE=13.5mg)。下面我们注意到必须考虑这种偏差。
▌临床比较
总体而言,与pH4时间较短的PPIs比较时,沃诺拉赞更有效(例如,在治疗消化性溃疡,非或轻度糜烂性食管炎时),沃诺拉赞和PPIs的结果通常是非劣效性的。相反,pH4时间较长的PPIs效果更佳(例如,治疗严重糜烂性食管炎时),沃诺拉赞的这种优势发生在与较低pH4时间的PPIs相比时。在治疗非糜烂性食管炎或洛杉矶分级A/B级食管炎时,PPIs与沃诺拉赞的治疗结果相似。例如,兰索拉唑30mg(27mg OE)与沃诺拉赞(5、10、20或40mg每日一次)的剂量范围研究报告显示,二者治疗洛杉矶分级A/B级食管炎患者的结果相似(非劣效)。洛杉矶分级C/D级患者,兰索拉唑30mg(pH4时间约45%)与5或10 mg沃诺拉赞(pH4时间~60%)的治疗效果相似(例如,分别是87%对87.3%,86.4%),患者可在4周治愈。然而,当沃诺拉赞的使用剂量产生大于80%的pH4时间时,愈合增加至95%以上,也就是说,使用20mg沃诺拉赞(pH4时间为84%)为100%,使用40mg沃诺拉赞为96%(pH4时间为90%)。虽然未进行研究,但如果将20mg沃诺拉赞与埃索美拉唑或雷贝拉唑40 mg b.i.d进行比较,则可以达到预期类似的愈合效果(两者pH4时间均为~85%)。这些结果清楚地表明了判断与相对效力相关的结果的重要性。
经验表明,大多数胃食管反流病(GERD)患者都有非糜烂性疾病,每日一次低剂量PPI即可治疗。然而,更严重的糜烂性疾病(洛杉矶分级C或D级)需要更高水平的酸抑制(例如,更长的pH4时间)。大量随机研究表明,每日一次服用高剂量的PPI(例如每天一次60mg或更多的OE)优于低剂量PPI,但仅约5%的病例有效。当需要低抗分泌剂时,临床PPI可能优于沃诺拉赞,因为临床PPI剂量可在2.4mg至72mgOE范围内。当需要接近100%pH4时间时,优势将转向沃诺拉赞,用于严重糜烂性食管炎,胃肠道出血或幽门螺杆菌根除治疗。
▌沃诺拉赞与幽门螺杆菌根除治疗
最近,世界卫生组织(WHO)将幽门螺杆菌列为对人类健康构成最大威胁的16种抗生素耐药细菌之一。该公告是世卫组织改善抗生素管理和减少抗生素滥用运动的一部分。他们的宣布恰逢幽门螺杆菌共识指南的出版,试图克服由于抗生素耐药导致的日益严重的根除治疗失败。沃诺拉赞于2014年在日本被批准用于一线和二线幽门螺杆菌根除治疗。日本最初的治疗研究比较了沃诺拉赞20mg b.i.d.和兰索拉唑30mg b.i.d.分别与阿莫西林和克拉霉素的一线7天疗程的三联疗法。含PPI和沃诺拉赞的疗法对克拉霉素敏感的患者产生了高效和等效的结果。而对克拉霉素耐药的患者,其治愈率不同(治愈率分别为沃诺拉赞80%和兰索拉唑40%)。由于克拉霉素的耐药性,因此在三联疗法中功能性地去除了克拉霉素,该研究实际上由两种不同的方案组成(三联疗法和由P-CAB或PPI加阿莫西林组成的二联疗法),二者同时进行。因此,总体结果严重依赖于耐药菌株的比例。该初步研究还涉及了先前有消化性溃疡的患者。日本后续的研究已经治疗了“所有参与者”,但整体治愈率低于90%并且一直在下降。使用沃诺拉赞和PPI的敏感菌株的治愈率也低于原始试验。目前推荐的含沃诺拉赞的幽门螺杆菌根除疗法在药物,剂量或疗程方面尚未得到优化。所有最近的共识声明都建议使用含PPI的14天疗程的方案以得到最佳的效果,克服幽门螺杆菌的持久状态,使PPIs达到完全抗分泌活性(例如,7天疗程,完全活性仅达到3至4天)。即使在易感情况下,使用7天克拉霉素PPI三联疗法的治愈率仅约为90%。
沃诺拉赞-阿莫西林双重疗法可治愈大约80%的感染,无论其他药物的耐药性如何。这与先前使用PPI-阿莫西林双重疗法的研究一致,显示根除效果取决于抗分泌作用的程度和治疗疗程。目前日本使用沃诺拉赞克拉霉素三联疗法的治愈率已接近单用沃诺拉赞-阿莫西林双重治疗所达到的治愈率,克拉霉素的增加率仅为百分之几(图1)。因为大约80%的患者在不含克拉霉素治疗的情况下可被治愈,而沃诺拉赞,克拉霉素,阿莫西林三联疗法代表滥用抗生素,因为对于大多数患者,克拉霉素可产生副作用并促进人群中抗生素耐药形成。由于甲硝唑耐药在日本很少见,日本幽门螺杆菌研究小组已请求政府允许使用沃诺拉赞-甲硝唑-阿莫西林作为一线治疗方案。然而,这并不会消除抗生素滥用,因为80%的患者会不必要地接受甲硝唑。
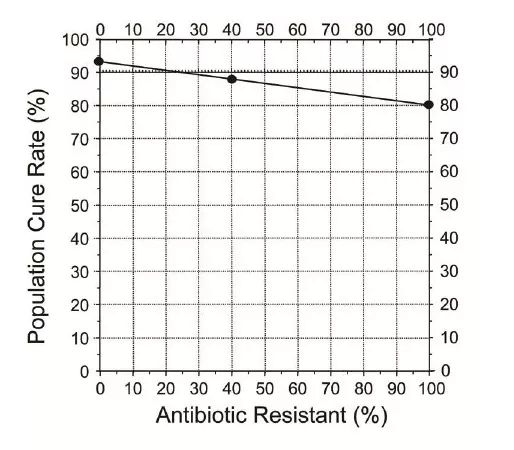
▲图1 | 克拉霉素耐药对7天疗程克拉霉素-沃诺拉赞三联疗法的整体治愈率的影响的实例。在该实例中,克拉霉素敏感和耐药的治愈率分别为93%和80%。克拉霉素耐药率为40%,总治愈率为87%。治疗特异性治愈率为:80%无论克拉霉素是否存在,克拉霉素的增量增加为7%,13%,尽管使用阿莫西林和克拉霉素也会失败。
解决这一难题有许多不相互排斥的选择。最好的方法可能是优化沃诺拉赞-阿莫西林双重疗法。高剂量PPI和阿莫西林已被证明在高度选择的人群中有效,但总体治愈率无法可靠地达到高于60%至80%。PPI代谢慢和胃肠炎患病率高的亚洲人群已经能够达到90%以上的治愈率,但这种类型的人群很难复制。尽管双重治疗中,对高治愈率至关重要的变量尚不清楚,但维持胃内pH值高于6,从而刺激幽门螺杆菌复制,以及足够的治疗疗程显得最为重要。同时也提出了维持阿莫西林较高的最小抑菌浓度(MIC)也很重要(例如,每6小时使用一次),但该假设尚未得到系统的评估并且发生了许多例外。幽门螺杆菌治疗的目标是可靠地治愈超过95%的感染患者并避免抗生素的滥用。应该使用PPI-阿莫西林方案先前丰富的经验,并且简单的析因设计可以快速提供答案。然后可以简化可靠的成功治疗方案(例如,14天,高剂量和低剂量的沃诺拉赞,以及b.i.d.,t.i.d.和q.i.d.阿莫西林,总剂量约为2至3克)。重点是确定在药物,配方,剂量和治疗疗程方面哪项最重要,而不是根据感知到的市场优势制定方案。
第二种方法是用沃诺拉赞和阿莫西林7至14天疗程的双重疗法(取决于增加的持续时间延长),剩余10-20%患者将接受适合该人群的最佳组合方案(例如,沃诺拉赞,阿莫西林,甲硝唑等),这将大大减少不必要的抗生素使用。第三种选择是在沃诺拉赞-阿莫西林双重疗法中添加非抗生素成分,如铋,益生菌等。理论上铋可能无效,但可将其作为氯氧化物或柠檬酸来发挥作用
▌预防内镜止血成功后再出血
已证实,每日口服一次,两次或三次PPIs的患者餐后胃内pH值>6是不可能实现的。 解决方法就是额外加入一种抑酸剂,使用沃诺拉赞或两者同时使用。沃诺拉赞的优点主要为快速起效,可抑制活跃和静息状态下的质子泵。单剂量研究表明,在第1天口服80mg剂量的沃诺拉赞即可以实现以上对胃内PH的要求。沃诺拉赞的使用,直接测试了保护血凝块这一理论的可行性,其将在内镜下成功止血后进一步减少或消除再出血。
▌沃诺拉赞与血清胃泌素及其他潜在警示
沃诺拉赞可有效减少酸分泌并刺激胃排空。血清胃泌素测量提供了一种简单的方法来测定其酸抑制的程度,胃酸缺乏症需要非常高的胃泌素水平。胃泌素增加从略高于正常值到超过1000 pg/mL变化,标准沃诺拉赞的剂量最可能反映药物影响酸分泌的可变性。在大多数与使用抗分泌药物相关的高胃泌素血症研究中,胃泌素水平不会持续升高,并在停止治疗后迅速恢复正常。在一项使用沃诺拉赞维持治疗食管炎52周研究中,得出了一些令人担忧,但尚未能解释的结果。在该研究中,曾治疗过食管炎的GERD患者接受了52周的10mg或20mg的沃诺拉赞维持治疗,患者的血清胃泌素水平呈显著渐进性增加(例如,从服药8周后的317±336pg/mL增加至777.6±678 pg/ml,每天20mg剂量;从291±219至514.5±435,每天10mg剂量)。在24周和52周时未发现胃神经内分泌细胞或胃蛋白酶原水平的显著变化。很难解释为什么胃泌素水平如此之高并且持续上升。从理论上讲,这些变化反映了酸抑制程度的增加。尚未有任何对胃窦和胃体粘膜组织学的详细分析。这一观察结果仍有待解释。
据推测,沃诺拉赞可能抑制位于肾髓质集合管中的肾HKα1-ATP酶,而传统的PPIs不发挥这种功能。这种抑制的重要性(如果有的话)尚未得到澄清。沃诺拉赞作为有效的抗分泌PPI制剂,可能会影响营养吸收(例如,铁和维生素B12)并减少酸屏障,导致肠道感染风险和肠道微生物组的变化,尤其对于那些在热带地区旅行的人。与其他有效的PPIs一样,这种影响很可能与酸抑制的有效性有关,但由于大多数数据都是类数据,异质性较大,因此尚未进行系统性研究。沃诺拉赞的使用风险是否与具有相似效力的传统PPIs不同仍有待研究。
▌总结
沃诺拉赞可被视为一种有效的长效PPI,与传统的PPIs相比具有一些潜在的优势。调整PPIs和沃诺拉赞的使用方式和剂量可以实现或多或少的酸抑制,从而达到所需要的酸抑制程度。目前克拉霉素和含有沃诺拉赞的幽门螺杆菌根除疗法可能会导致克拉霉素或甲硝唑的滥用。沃诺拉赞有望能够可靠地实现胃内pH>5甚至PH>6,使其可用于预防内镜下止血后复发出血或幽门螺杆菌根除治疗的佐剂,并能提高阿莫西林加一种抗分泌剂治疗的治愈率,沃诺拉赞也可有助于管理胰腺功能不全患者的脂肪吸收不良。目前使用的肠溶胰酶微珠倾向于从膳食中解离,并在通过小肠期间缓慢且不可预测地溶解,阻碍了酶和营养物的协调性排空。未受保护的酶与营养素混合均匀且一起排空,但在pH为4或更低时酶是失活的。沃诺拉赞能够在长时间内可靠地维持胃内pH>4,这样就可以常规使用非肠溶性酶。作用时间长,良好的生物利用度,酸稳定性以及可抑制活跃和静息状态下的质子泵,种种这些表明沃诺拉赞可用于病情难以管理的患者,例如Roux-en-Y胃旁路手术或其他减肥手术的患者,他们缺乏胃窦胃泌素的释放,胃排空迅速,小肠肠溶包衣PPIs溶解和吸收的吸收面积小,传统的抗分泌治疗较为困难。目前,当需要比60-70mg奥美拉唑当量b.i.d所获得更多的酸抑制时,沃诺拉赞起着重要而独特的作用。然而,这种情况很少见,除了Zollinger-Ellison综合征,通常使用疗程较短。沃诺拉赞是否合适且长期安全,甚至终身使用,仍有待确定。
原始出处:
Graham DY, Dore MP, Update on use of vonoprazan: a competitive acid blocker (P-CAB), Gatroenterology (2018).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#AZ#
30
#沃诺拉赞#
38
#AST#
27
#GAS#
26
#Gastroenterol#
30
#Gastroenterology#
28