Lancet Neurol:荷兰心房颤动患者抗凝相关脑出血后阿匹沙班与不抗凝的比较(APACHE-AF)
2021-10-28 Naomii MedSci原创
心房颤动患者在服用抗凝剂期间发生脑出血,无论是分配给阿匹沙班还是为了避免抗凝,随后发生非致命性中风或血管死亡的年度风险都很高。
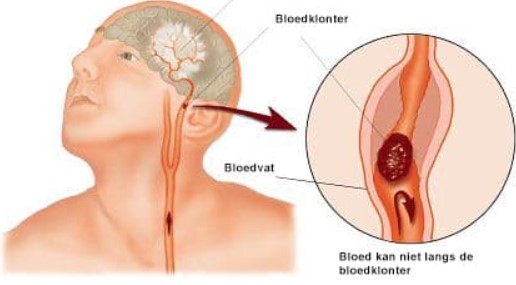
对于在抗凝相关脑出血中幸存下来的房颤患者,是否重新启动抗凝以预防中风复发和系统性血栓栓塞是一个长期而紧迫的临床难题。长期以来,医生一直不愿推荐口服抗凝治疗,只有少数患者恢复治疗,而且往往在脑出血后几个月恢复治疗。最近,观察性研究提供了支持重新开始抗凝的论据。在患有心房颤动的抗凝相关脑出血的幸存者中,恢复口服抗凝与较低的死亡风险及比避免抗凝更好的功能结果相关,这些关联在非脑叶和脑叶出血的患者中相似,尽管脑叶内出血的患者比非脑叶出血的患者有更高的再发脑出血风险。
然而,这些观察性研究的结果可能与适应症相混淆,大多数接受抗凝治疗的患者都使用维生素K拮抗剂。非维生素K拮抗剂口服抗凝剂被称为直接口服抗凝剂(DOAC),在房颤患者短暂性脑缺血发作和缺血性卒中后的一级预防和二级预防中,出血性并发症的风险低于维生素K拮抗剂。因此,DOAC可能是更安全的选择,尤其是在抗凝相关脑出血的患者中。因此,指南没有提供强有力的建议,建议抗凝相关脑出血的患者(如果有的话)应该恢复抗凝。
对于在抗凝相关脑出血中幸存下来的心房颤动患者,必须决定重新开始抗凝还是永久避免抗凝是预防中风和其他血管事件复发的最佳长期策略。近日,研究人员在APACHE-AF的研究中,评估了接受阿匹沙班治疗的此类患者与避免抗凝治疗时的非致命性卒中或血管死亡的比率,以便为更大规模试验的设计提供依据。
APACHE-AF是在荷兰的16家医院进行的一项前瞻性、随机、开放标签的2期试验,进行了蒙蔽终点评估。脑出血患者在接受心房颤动抗凝治疗期间幸存下来的患者在出血后7-90天符合纳入标准。参与者的CHA2DS2-VASc评分至少为2分,改良Rankin量表(MRS)评分为4分或更低。参与者被随机分配(1:1)接受口服apixaban(每天两次5毫克或减少剂量每天两次2.5毫克)或避免抗凝(口服抗血小板药物可以由治疗医生自行决定),根据随机避免抗凝的参与者开始或停止抗血小板治疗的意图进行分层,并根据年龄和脑出血部位将其降至最低。在至少6个月的随访中,主要结果是非致命性中风或血管性死亡(以先发生者为准)的组合,在意向治疗人群中使用Cox比例风险模型进行分析。APACHE-AF在ClinicalTrials.gov(NCT02565693)和荷兰试验登记处(NL4395)注册,该试验在所有参与网站关闭注册。

- 在2015年1月15日至2020年7月6日期间,共招募了101名脑出血后患者(中位年龄78岁[IQR 73-83];55[54%]男性和46[46%]女性;100[99%]白人和1[1%]黑人),中位年龄46天(IQR 21-74)。50人接受阿匹沙班治疗,51人避免抗凝(其中26人(51%)开始抗血小板治疗)。无一例失访。中位随访时间为1.9年(IQR 1·0-3·1;222人年);
- 13名(26%)被分配给阿匹沙班的参与者(年度事件发生率为12.6%[95%CI 6·7-21.5])和12名(24%)被分配为避免抗凝的参与者发生了非致命性中风或血管死亡(11.9%[95%CI 6·2-20.8];调整后的风险比为1.05[95%CI 0·48-2.31]);
- 在被分配给阿匹沙班的50名参与者中有29名(58%)发生了非结局事件的严重不良事件,在51名被分配到避免抗凝的参与者中有29名(57%)发生了严重不良事件。
心房颤动患者在服用抗凝剂期间发生脑出血,无论是分配给阿匹沙班还是为了避免抗凝,随后发生非致命性中风或血管死亡的年度风险都很高。该研究强调了需要规模足够大的随机对照试验,以便识别重新开始抗凝可能有益或有害的亚组。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言

















#Neurol#
44
#APACHE#
29
#Lancet#
45
#APA#
37
#心房#
38