Immunity:以一己之力对抗慢性病毒感染
2017-08-16 欧阳沐 生物通
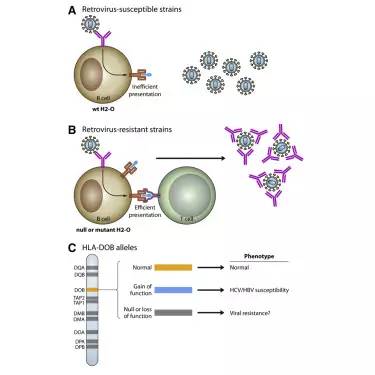
近年来,芝加哥大学的微生物学、免疫学、遗传学家Tatyana Golovkina博士一直在试图解决一个棘手问题:为什么有些人和动物能抵御病毒持续感染,而其他人却不行呢? I/LnJ品系小鼠特别擅长控制病毒感染。它们能生产对抗多种不同属逆转录病毒的特异性抗体。 Golovkina就很好奇,所以她开始在I/LnJ小鼠身上寻找负责提高免疫反应的基因。本周《Immunity》发表了她的最新文章
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Immunity#
35
#慢性病#
29
认真学习,不断进步,把经验分享给同好。点赞了!
54
非常棒的研究
54
学习了,谢谢
54