Int J Cardiol:女性支架内血栓形发病率、影响因素和对死亡率的临床影响!
2018-04-17 xing.T MedSci原创
在这一大规模的妇女合并分析中,明确的ST较为罕见,但与死亡风险有关,其早期达到高峰,并随着时间的推移迅速减弱。年龄较小、糖尿病、NSTEMI和支架直径被认为是ST的预测因素。
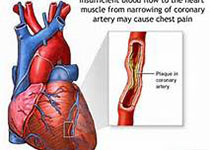
女性支架血栓形成(ST)的预测和临床结果还没有得到很好的调查。近日,心血管领域权威杂志International Journal of Cardiology上发表了一篇研究文章,该研究旨在确定经皮冠状动脉介入治疗(PCI)的女性ST的预测因素及其对死亡率的影响。
研究人员纳入了26个DES随机试验的女性患者层面的数据,并进行汇总。研究人群根据有无ST进行分层。Cox比例风险模型被用来确定ST的预测因素,为了分析ST对死亡率的时间影响,ST作为时间更新协变量的Cox回归被用于分析。
11557例患者接受PCI并植入了支架,在3年的中位随访期间,明确ST发生为105例(0.9%)。ST的独立预测因素为年龄(HR每年降低为1.03,95%可信区间为1.0-1.05;P = 0.041)、糖尿病(HR为2.25,95% CI为1.27–3.99;P = 0.005)、就诊时非ST段抬高型心肌梗死(NSTEMI)(HR为1.97,95%CI为1.04–3.75;P = 0.037)和支架直径(每3.76毫米减少的HR为3.76,95%CI为1.66–8.53;P=0.002)。与无ST的女性相比,在前7天、8-30天以及超过30天因ST死亡的调整后风险比分别为115.81(95%CI为68.96–194.47)、37.44(95%CI为17.31–80.98)以及3.54(95%CI为2.20–5.69)。
在这一大规模的妇女合并分析中,明确的ST较为罕见,但与死亡风险有关,其早期达到高峰,并随着时间的推移迅速减弱。年龄较小、糖尿病、NSTEMI和支架直径被认为是ST的预测因素。
原始出处:
Laura S.M. Kerkmeijer,et al. Incidence, determinants and clinical impact of definite stent thrombosis on mortality in women: From the WIN-DES collaborative patient-level pooled analysis.International Journal of Cardiology.2018. https://doi.org/10.1016/j.ijcard.2018.04.047
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床影响#
0
#支架内血栓#
33
#发病率#
21
#Cardiol#
22
医学女性与男性治疗的不同之处
45
谢谢分享
54
#影响因素#
20
学习了
53
好
48
不错的文章值得拥有
57