J Thorac Oncol:掀起免疫治疗NSCLC继发耐药的神秘面纱
2018-04-08 肿瘤资讯编辑部 肿瘤资讯
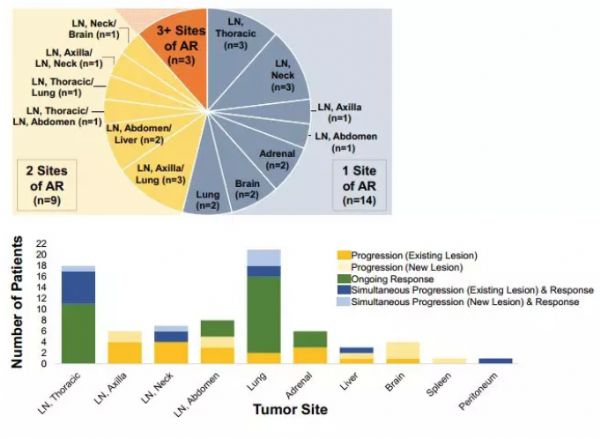
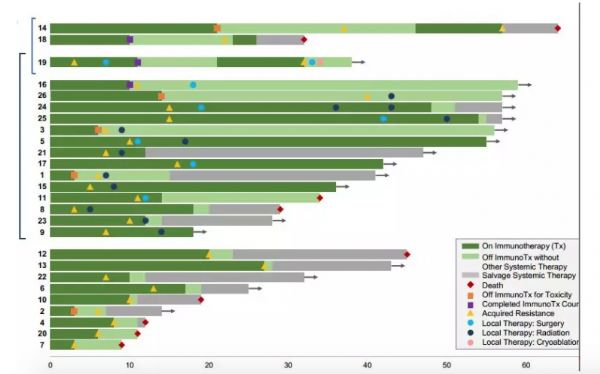
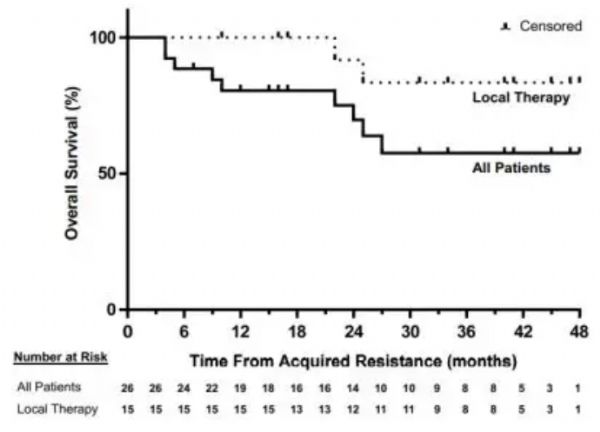
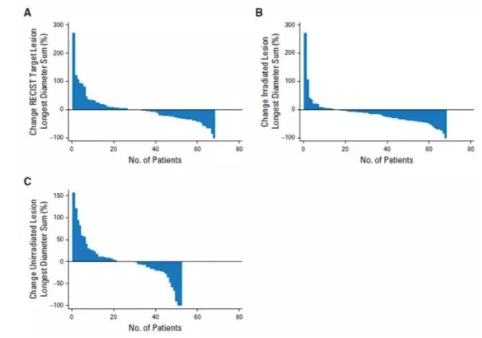
免疫检查点抑制剂治疗NSCLC可谓全面开花,但继发耐药研究较少。2018年3月22日JTO在线发表来自耶鲁癌症中心的研究,免疫治疗NSCLC继发耐药特点:进展部位以淋巴结为主,寡进展,局部治疗是处理继发耐药的重要手段。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#继发#
19
#THORAC#
25
#Oncol#
20
学习了
68
学习了很多先进的医学知识
38
我觉得非常好
52