Expert Opin Biol Ther :Suckinumab治疗掌趾银屑病
2022-08-30 医路坦克 MedSci原创
掌趾银屑病通常是指主要影响手掌和/或脚底的过度角化性银屑病,我们在这里描述了临床实践中使用Suckinumab治疗的患者的结果。

掌趾银屑病通常是指主要影响手掌和/或脚底的过度角化性银屑病,有或没有其他身体部位的累及。据报道,在流行病学研究中,这种表型在银屑病患者中的患病率>10%,其特征是红斑和角化斑块,有或没有裂隙,可以延伸到手腕和足底表面的边缘。掌底银屑病给患者带来的负担是巨大的,主要是由于功能障碍、疼痛和皮损的可见性。这导致与身体其他部位的银屑病患者相比,掌趾银屑病患者的健康相关生活质量(QOL)受到更大的损害。在这种银屑病表型中,体表面积(BSA)受影响的程度通常小于5%,而且低于其他银屑病类型。然而,与受累部位较大但难度较小的患者相比,患者可能报告更大的残疾、疼痛和生活质量损害。掌趾型银屑病的治疗往往具有挑战性,而且对银屑病的常规治疗方法也难以接受。生物制品已被证明是有效的,耐受性良好。
Suckinumab是一种完全人源的IgG1单抗,可与白介素17A结合,从而阻断在银屑病发病机制中起关键作用的炎症途径。值得注意的是,据报道,IL-17A在掌底脓疱性银屑病患者的手掌和足底表达增加。2期和3期临床试验的结果已经证明了Suckinumab治疗中重度银屑病的有效性和良好的安全性。Suckinumab也被证明可以改善掌底银屑病。现实世界中使用Suckinumab治疗掌趾银屑病的证据有限。
因此,我们在这里描述了临床实践中使用Suckinumab治疗的患者的结果。
方法:这是一项在意大利的7家皮肤科诊所接受Suckinumab(300毫克,皮下注射)治疗的掌趾银屑病患者的真实、回顾性、观察性研究。根据治疗过程中银屑病面积和严重程度指数(PASI)和掌跖(Pp)PASI的变化以及104周以上的安全性和耐受性问题来评估治疗效果。
结果:43名患者开始使用Suckinumab治疗。以前的治疗包括局部和系统治疗;一半的患者已经尝试了一种或多种生物制剂。Suckinumab迅速显著改善了平均PASI,16周时下降了78.2%。平均ppPASI也有显著改善,但幅度更小,在16周和104周时分别下降了55.0%和79.3%。大约一半的患者在40周时皮肤完全清除。Suckinumab耐受性良好,没有相关治疗相关不良事件的报告。
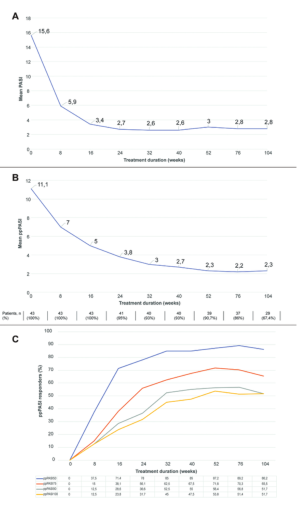
Suckinumab对掌足部银屑病患者104周绝对PASI(A)、绝对ppPASI(B)和ppPASI 50、75、90和100反应率(C)的影响。
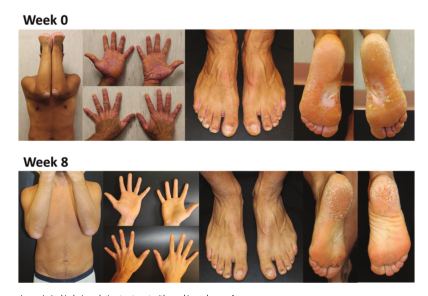
1例Suckinumab治疗过程中银屑病皮损的变化。

2例Suckinumab治疗过程中银屑病皮损的变化。
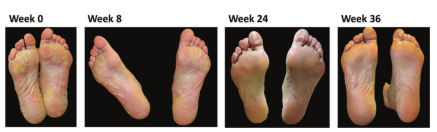
银屑病皮损在接受Suckinumab治疗过程中的变化:例3。

Suckinumab治疗期间银屑病皮损的变化:例4(A)和5(B)。
结论:研究发现表明,对于临床实践中遇到的手掌和脚底受累的难以治疗的银屑病患者,Suckinumab是一种成功的治疗选择。我们的非选择患者群体中描述的Suckinumab作用的有效性、耐受性和作用时间与临床试验对照设置中报告的相一致。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
38
#mAb#
0
#Bio#
32
#Biol#
35