端粒长度被认为是衰老的潜在生物学标志。这些重复的核苷酸序列,连同相关的蛋白质复合体,在染色体末端形成一个“帽”,保护它们免受损伤。由于细胞的复制机制不能完全复制染色体的末端,每次分裂都会丢失50-100对碱基对。因此,随着细胞年龄的增加,端粒磨损也会发生。极短的端粒触发细胞死亡或复制性衰老,或偶尔持续分裂、突变和基因畸变。从流行病学的角度来看,较短的白细胞端粒长度(LTL)与一些衰老相关的疾病,包括阿尔茨海默病、癌症和冠状动脉疾病有关。端粒长度部分可遗传,与性别、种族和父亲年龄有关,但也与环境和生活方式因素有关,包括运动、吸烟和饮酒。
端粒长度被认为是生物衰老的标志,而酒精对端粒长度的影响尚不清楚。牛津大学大数据研究所纳菲尔德系人口健康部进行了迄今为止最大的观察性研究(245354名英国生物库参与者),并将研究结果与孟德尔随机化(MR)估计进行了比较。研究结果发表在Molecular Psychiatry。
双样本MR使用了472,174名参与者的数据,这些参与者参加了最近的端粒长度全基因组关联研究(GWAS)。根据与酒精消费(n = 941,280)和酒精使用障碍(n = 57,564例)的相关性选择遗传变异。非线性MR采用英国生物银行个人数据。
结果如下:
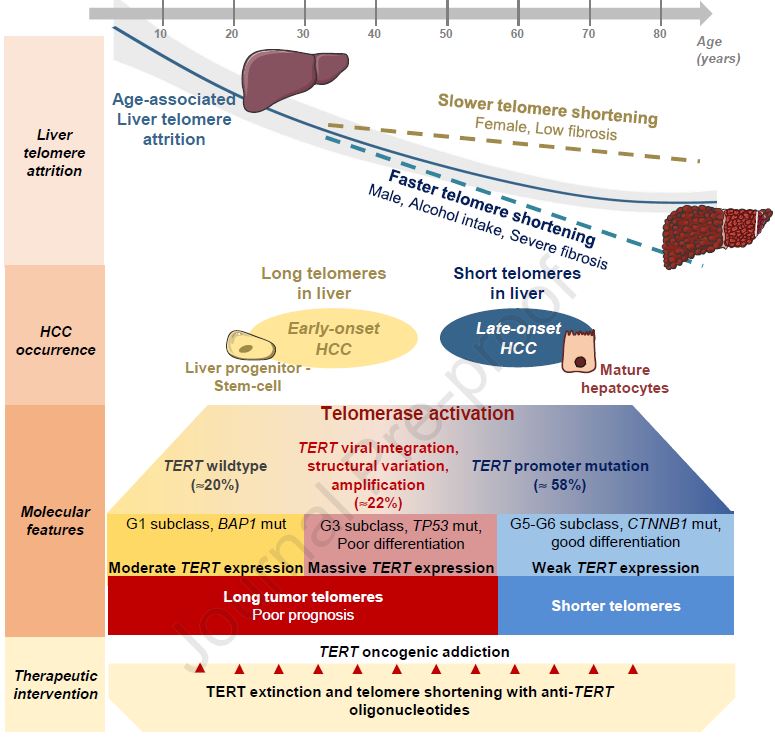
1. MR分析表明酒精性状(在AUD中更明显)与端粒长度之间存在因果关系。较高的遗传预测AUD(反向方差加权(IVW) β =−0.06,95%置信区间(CI):−0.10 ~−0.02,p = 0.001)与较短的端粒长度相关。与基因预测的每周饮酒有较弱的相关性(IVW β =−0.07,CI:−0.14至−0.01,p = 0.03)。
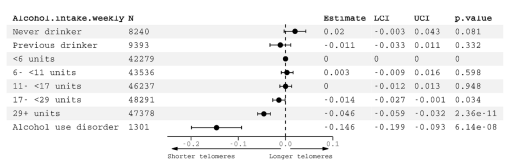
图1.白细胞端粒长度的观察相关性
2. 不同方法的结果是一致的,与吸烟无关。非线性分析表明酒精和端粒长度之间存在潜在的阈值关系。
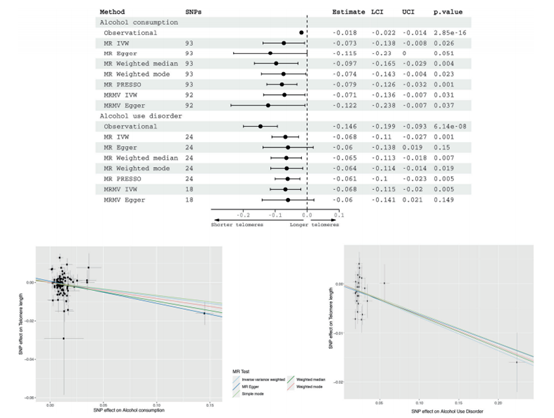
图2.对于基因预测饮酒和饮酒障碍与端粒长度之间的关系,采用顶级多变量调整观察估计(在245354名UKB参与者中)和双样本孟德尔随机估计(双样本设计)。
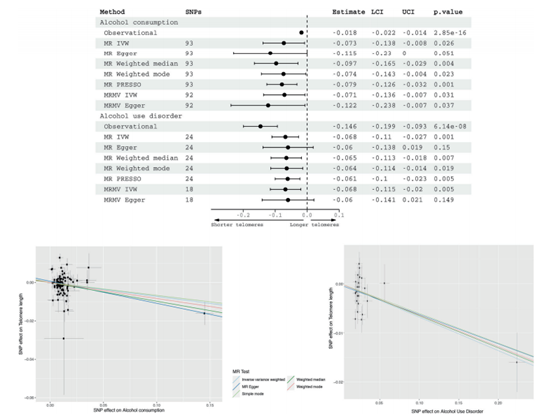
图3.基因预测饮酒与端粒长度之间的非线性孟德尔随机估计,按周酒精摄入量分层(无静脉注射)。
总之,发现了酒精性状、遗传预测的酒精性状和端粒长度之间的关联。非线性分析表明,饮酒阈值对影响端粒长度可能是必要的。这些发现支持酒精,特别是在依赖水平上,是端粒长度的因果决定因素。对估计方法的假设进行多重敏感性分析,为估计方法的合理性提供了一定程度的可信度。这些发现为临床医生试图说服患者酒精的有害影响提供了另一条信息。端粒缩短被认为是一些老年疾病如阿尔茨海默病的因果风险因素。此外,酒精的剂量也很重要——即使是减少饮酒也会有好处。
原文出处
Alcohol consumption and telomere length: Mendelian randomization clarifies alcohol’s effects
https://www.nature.com/articles/s41380-022-01690-9.pdf
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Psychiatry#
52
学习
32
学习学习
34
#期刊论坛##学习#
58
不错的文章
45
酒精是一级致癌物,少喝为妙。
33