European Radiology:互动专用培训计划在膀胱MR VI-RADS分数中的价值
2022-08-23 shaosai MedSci原创
近年来,磁共振成像(MRI)已成为临床上一种可靠和准确的BCa诊断和分期的工具。特别是膀胱成像-报告和数据系统(VI-RADS)评分的制定,为膀胱MRI的获取、解释和报告提供了系统化和标准化的方法。
据统计,膀胱癌(BCa)是全球范围内第10大最常见的恶性肿瘤,全球约有55万新发病例和20万死亡病例。
近年来,磁共振成像(MRI)已成为临床上一种可靠和准确的BCa诊断和分期的工具。特别是膀胱成像-报告和数据系统(VI-RADS)评分的制定,为膀胱MRI的获取、解释和报告提供了系统化和标准化的方法以区分肌肉浸润性和非肌肉浸润性膀胱癌,目的之一是减少不同中心之间的结果异质性。
有趣的是,除了高诊断性能外,VI-RADS评估评分在专家和无经验的放射科医生之间都显示出相当大的评分者间一致性。随着放射学技术的快速发展,医学院和住院医师项目必须采用新的学习方法以便对放射学课程的实施进行实质性的改变。
近日,发表在European Radiology杂志的一项研究评估了放射科住院医师在互动的专门培训项目中使用VI-RADS评分判析膀胱MRI的学习曲线。

有三位在膀胱MRI方面经验不多的放射科住院医师担任读片员。他们在3个月内对200份研究报告进行了盲评,分为4个子集,每集50例。2个月后,对第一个子集进行了重新评估,总共评估了250个病例。本研究提供了一个互动的培训项目,包括教育课程和基于病例的练习。学习曲线是通过将平均一致度绘制成每批正确评价的比率来构建的。通过卡帕统计学和ROC分析,进行了阅读者之间的一致性和诊断性能分析。
关于VI-RADS评分的一致性,读者1在培训前和培训后对同一组病例的评估的卡帕差异为0.555至0.852,读者2为0.522至0.695,读者3为0.481至0.794。使用VI-RADS≥3作为肌肉侵犯的分界线,敏感性为84%至89%,特异性为91%至94%,而AUCs为0.89(95% CI:0.84, 0.94)至0.90(95% CI:0.86, 0.95)。子集1和5的平均评估时间从5.21±1.12分钟减少到3.52±0.69分钟。在子集1和5中,平均信心等级从3.31±0.93提高到4.21±0.69。
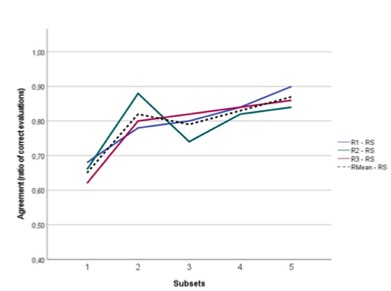
图 读者对VI-RADS评分的学习曲线,基于每个图像子集的读者和参考标准之间一致的评价比率。R1,读者1;R2,读者2;R3,读者3;RS,参考标准;RMean,读者的平均值
本研究表明,关于膀胱MRI和VI-RADS评分的互动式专用读者教育计划与读者的诊断表现随着时间的推移而显著增加有关。这些发现为进一步改善和塑造未来的研究计划和放射学课程提供了参考依据。
原文出处:
Miguel Correia da Silva,Martina Pecoraro,Martina Lucia Pisciotti,et al.The learning curve in bladder MRI using VI-RADS assessment score during an interactive dedicated training program.DOI:10.1007/s00330-022-08766-8
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#PE#
51
#ADS#
36
#RADS#
43