European Radiology:FROC模型和双参数VI-RADS对膀胱尿路上皮癌分期和分级的评价
2022-01-11 shaosai MedSci原创
膀胱癌是全球第十大最常见的癌症,2018年有54.9万新发病例,约20万人死亡。大多数膀胱癌在组织学上被归类为尿路上皮癌,其治疗方案主要根据浸润深度和组织学等级来决定。
 膀胱癌是全球第十大最常见的癌症,2018年有54.9万新发病例,约20万人死亡。大多数膀胱癌在组织学上被归类为尿路上皮癌,其治疗方案主要根据浸润深度和组织学等级来决定。对于非肌层浸润性膀胱癌(NMIBC;T1期或更低)患者,通常推荐经尿道膀胱肿瘤切除术(TURBT),而更具侵袭性的肌层浸润性膀胱癌(MIBC;T2期或更高)经常需要进行根治性膀胱切除术、辅助化疗或两者同时进行。因此准确评估有无肌层浸润和肿瘤细胞分化程度,不仅对选择最佳治疗方案至关重要,而且对低风险的NMIBC患者避免不必要的侵入性治疗也十分重要。
膀胱癌是全球第十大最常见的癌症,2018年有54.9万新发病例,约20万人死亡。大多数膀胱癌在组织学上被归类为尿路上皮癌,其治疗方案主要根据浸润深度和组织学等级来决定。对于非肌层浸润性膀胱癌(NMIBC;T1期或更低)患者,通常推荐经尿道膀胱肿瘤切除术(TURBT),而更具侵袭性的肌层浸润性膀胱癌(MIBC;T2期或更高)经常需要进行根治性膀胱切除术、辅助化疗或两者同时进行。因此准确评估有无肌层浸润和肿瘤细胞分化程度,不仅对选择最佳治疗方案至关重要,而且对低风险的NMIBC患者避免不必要的侵入性治疗也十分重要。
在临床上,TURBT是确定肌肉浸润性和组织学等级的标准方法。然而,据报道,在高达25%的肌层浸润性膀胱癌中,肿瘤可能被低估,并且由于取样错误,高达15%的肿瘤会出现不准确的分级。这些局限性以及TURBT手术的高成本和侵入性,表明非常需要一种无创的、更准确的成像技术来协助对膀胱尿路上皮癌进行分期及分级。
膀胱成像-报告和数据系统(VI-RADS)的引入为临床上的对膀胱癌的规范化评估及判读提供了基础。现阶段,分阶微积分(FROC)模型已在临床上的多个方面应用及认可。FROC模型提供了三个参数:扩散系数D(单位:μm2/ms),空间分阶导数β(无量纲)以及空间参数μ(单位:μm)。当与VI-RADS结合时,该模型也可以提高诊断性能。
近日,发表在European Radiology杂志的一项研究探讨了在高b值下使用DWI与FROC模型对尿路上皮癌进行分期和分级的可行性,同时比较了FROC参数与ADC的性能,并研究了当FROC参数与简化版的VI-RADS相结合时提高诊断性能的情况,为膀胱癌的术前无创性准确评估提供了强有力的支持。
本项前瞻性研究纳入了58名患有膀胱尿道癌患者。使用FROC模型分析了以16个b值(0-3600s/mm2)获取的扩散加权图像。三个FROC参数,D、β和μ,被用于划分NMIBC和MIBC,并用于肿瘤分级。基于单个FROC参数及其组合进行了受试者工作特性(ROC)分析,然后与基于T2加权图像和DWI的表观扩散系数(ADC)和双参数VI-RADS进行比较。
MIBC组的D和μ明显低于NMIBC组(各P = 0.001),D、β和μ在高等级肿瘤中都表现出明显低于低等级肿瘤(P ≤ 0.011)。D、β和μ的组合对区分NMIBC和MIBC产生了最高的特异性(85%)、准确性(78%)和ROC曲线下的面积(AUC,0.782),对肿瘤分级产生了最好的敏感性(89%)、特异性(86%)、准确性(88%)和AUC(0.892),这些都优于ADC。FROC参数与双参数VI-RADS的组合将AUC从0.859提高到0.931。
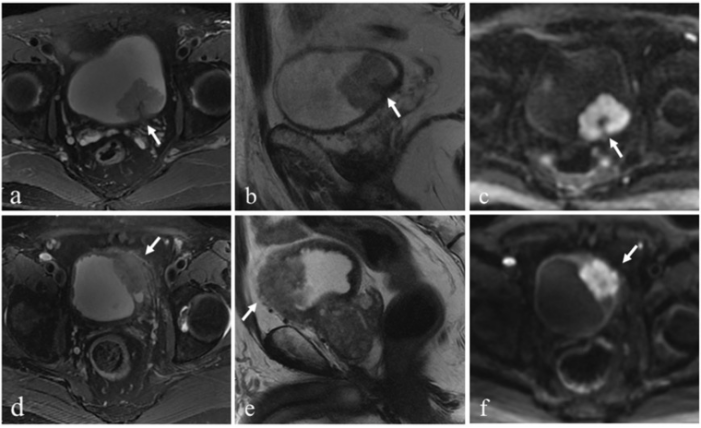
图 上排:NMIBC患者。轴位(a)和矢状位(b)T2加权图像显示左后壁的外生性肿瘤,有低信号的柄(箭头)和完整的固有肌层线,表明T2加权成像评分为2。b=1000s/mm2的扩散加权图像(c)显示一个高信号强度的肿瘤,有一个低信号强度的柄(箭头),表明DWI评分为2。下图 行:MIBC患者。轴位(d)和矢状位(e)T2加权图像显示左侧壁上的肿瘤,并延伸至周围脂肪(箭头),表明T2加权成像评分为5。b=1000s/mm2的弥散加权图像(f)显示高信号强度的肿瘤延伸至周围脂肪(箭头),表明DWI评分为5分。最终双参数VI-RADS评分为5分。
本研究证明,无论是单独还是联合应用FROC模型参数,该模型均可用于划分NMIBC和MIBC以及低级和高级膀胱尿上皮癌。FROC模型参数可以超越传统的ADC,提高双参数VI-RADS的诊断性能。随着进一步的验证,FROC扩散模型可能成为一个潜在的基于成像的工具,以协助组织病理学和VI-RADS来描述膀胱尿路上皮癌的特征及分级。
原文出处:
Cui Feng,Yanchun Wang,Guangyu Dan,et al.Evaluation of a fractional-order calculus diffusion model and bi-parametric VI-RADS for staging and grading bladder urothelial carcinoma.DOI:10.1007/s00330-021-08203-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#膀胱尿路上皮癌#
55
#RADS#
41
#ROC#
40
#ADS#
47
#PE#
35
#评价#
33
#上皮癌#
45