APASL 2013:恩替卡韦长期抗病毒治疗降低HCC风险
2013-07-19 MedSci 中国医学论坛报
国内外最新慢性乙肝(CHB)治疗指南均将“通过抗病毒治疗阻断肝脏疾病进展,减少肝硬化、失代偿期肝病和肝细胞癌(HCC)的发生,从而改善生存和生活质量”作为CHB治疗的最终目标。 因此,恩替卡韦(ETV)等强效核苷(酸)类药物(NUC)长期治疗是否减少或阻断HBV相关HCC的发生,成为乙肝治疗领域最受关注的话题之一。近日,在2013亚太肝病研究学会(APASL)年会上,多位国际知名专家报告了这方面的
国内外最新慢性乙肝(CHB)治疗指南均将“通过抗病毒治疗阻断肝脏疾病进展,减少肝硬化、失代偿期肝病和肝细胞癌(HCC)的发生,从而改善生存和生活质量”作为CHB治疗的最终目标。 因此,恩替卡韦(ETV)等强效核苷(酸)类药物(NUC)长期治疗是否减少或阻断HBV相关HCC的发生,成为乙肝治疗领域最受关注的话题之一。近日,在2013亚太肝病研究学会(APASL)年会上,多位国际知名专家报告了这方面的最新研究成果,为解答前述问题提供了更为充分的证据。
HBV感染与HCC发生密切相关
南方医科大学南方医院 侯金林
HCC的发生率和死亡率分别居全球第5位和第4位。世界范围内,半数以上的HCC与乙型肝炎病毒(HBV)感染有关,在HBV感染高流行的亚洲,这一比例高达70%~80%。
HBV与HCC的密切关联已被基础研究和流行病学数据证实。HBV的致癌机制是多方面的,感染病毒的肝细胞因慢性炎症受损、进而导致纤维化和肝硬化的过程中,宿主DNA可发生突变;HBV基因组整合入宿主DNA导致的染色体不稳定可引起基因表达和功能的改变;HBx蛋白通过干预细胞转录和信号传导在HBV致癌中发挥重要作用。
中国台湾REVEAL研究从流行病学角度证实HBV与HCC的相关性。通过对3653例乙肝表面抗原(HBsAg)阳性患者长达13年的随访,发现高病毒载量与HCC死亡风险增加有关,基线HBV DNA≥104~5 拷贝/毫升可能是患者发展为肝硬化和HCC的独立预测因素。
ETV是抗HBV治疗成功的优选之一
NUC的诞生为治疗HBV感染提供了有力武器。着眼于抗病毒疗效、低耐药、长期安全性和依从性选择初始治疗药物,是CHB长期管理成功及远期获益最大化的关键。ETV因强效抗病毒、高耐药基因屏障及良好的安全性和依从性,被权威指南推荐为CHB治疗的一线或优选治疗药物之一。
ETV临床试验结果显示,ETV治疗5年,94%的患者HBV DNA<300 拷贝/毫升;长期治疗可逆转肝纤维化,减少肝硬化患者进展为失代偿、HCC或肝相关死亡的发生率。耐药发生可抵消已取得的抗病毒疗效,ETV拥有高耐药基因屏障,6年耐药发生率仅为1.2%。在NUC治疗过程中备受关注的乳酸酸中毒和骨密度降低等安全性方面的问题,ETV的发生率极低。
ETV在临床实践中的疗效和安全性与全球临床试验数据一致。REALM研究是迄今全球最大规模的ETV治疗CHB的临床实践研究,中国研究包括50家中心5333例患者,64%为乙肝e抗原(HBeAg)阳性,ETV 1年和长期(192周)治疗后HBV DNA<50 IU/ml的比例均远高于其他NUC,而安全性相当。中国香港5年队列研究包括222例CHB初治患者,90%为HBeAg阳性,结果显示,ETV治疗5年后HBV DNA<20 IU/ml的比例为97%,HBeAg血清学转换率为67%,累计耐药发生率仅为1.2%。意大利队列(5年)研究证实了ETV单药长期治疗对欧洲患者的良好疗效。一项欧洲多中心VIRGIL研究包括10个欧洲中心的372例CHB初治和经治患者,其中89例为肝硬化患者(9例为失代偿期),发现对ETV治疗有应答者的疾病进展风险较无应答者显著降低70%。
ETV长期治疗与HCC:真实实践证据
阻断疾病进展至HCC是CHB长期治疗的重要目标之一。新近的多项研究证实,有效的抗病毒治疗虽不能完全阻止HCC发生,但可显著降低HCC的远期发生风险。在现有NUC中,拉米夫定(LAM)虽可降低HCC风险,但高耐药发生率可能抵消其长期获益; ETV不仅在抗病毒作用方面拥有丰富的循证医学证据,在降低HCC发生等方面亦积累了多项有力的证据,而替诺福韦(TDF)治疗对HCC发生风险的影响目前数据相对较少。
预防HCC发生
中国台湾和日本学者完成的研究均显示ETV长期治疗可显著降低HCC风险。在2013 欧洲肝脏研究学会(EASL)年会上报告的台湾研究纳入ETV治疗患者706例,均为HBeAg阴性、肝硬化且无HCC病史,并纳入196例患者作为历史性对照,随访结果显示,ETV组的HCC发生率显著低于对照组(12%对48.2%),ETV是HCC风险降低的唯一风险因子(HR为0.391)。
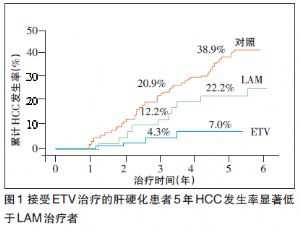
日本虎门医院在2013 年APASL年会上报告的研究以未接受NUC治疗(当时尚无NUC)的过往患者为对照组,结果显示,与对照组相比,ETV治疗可使5年HCC发生风险降低超过60%(HR为0.37),以肝硬化患者获益更明显。且接受ETV治疗的肝硬化患者5年HCC发生率显著低于LAM治疗者(7%对22.2%,图1)。应用HCC风险评分工具对患者进行分层后显示,高危患者接受ETV治疗后的HCC风险降低最明显。
韩国学者报告,ETV治疗应答可显著降低HCC风险,即使在进展期肝硬化患者中亦有显著获益。研究纳入的患者中32.1%(104/324例)为失代偿期肝硬化,结果显示,与ETV治疗无应答者相比,对ETV有应答者发生HCC的比例显著降低 [15%(42/278)对37%(17/46)]。
来自希腊的HepNet研究显示,ETV在降低HCC风险方面优于LAM(至少在非肝硬化患者中)。该研究的ETV与LAM治疗队列分别包括321和818例患者,60个月随访结果显示,两组的HCC累计发生率有显著差异(2.8%对5.6%)。
改善HCC患者生存
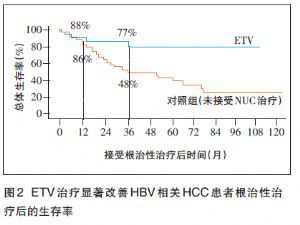
日本学者报告,初始选择ETV治疗可显著改善HBV相关HCC患者根治性治疗后的生存率,生存率提高60%以上(HR为0.33)。该研究纳入HCC患者70例,35例接受ETV治疗,35例未接受任何NUC治疗。ETV治疗组与对照组患者的1年和3年生存率分别为88%对86%、77%对48%,120周后ETV组和对照组分别有6和24例患者死亡(图2)。多因素回归分析显示,ETV治疗和肿瘤分期是影响生存的独立风险因子。
韩国首尔大学医院学者报告的一项历时4年的前瞻性研究显示,对于合并HCC的CHB患者,根治性治疗后给予ETV治疗可降低HCC复发风险,改善无疾病生存(DFS)。患者分为NUC治疗组(48例,接受ETV和其他NUC者分别为29和19例)和非治疗组(58例)。结果显示,ETV治疗较非NUC治疗组可显著降低HCC复发风险(比值比为 0.454)。
HCC风险预测工具的价值
基于对HBV与HCC密切关系的深入认识,目前已建立了几种HCC风险预测工具(例如REACH-B、GU-HCC评分以及GAG-HCC),并一致纳入了基线病毒载量这一重要参数。
香港中文大学今年发表的在一组1531例接受ETV治疗的CHB患者中进行的回顾—前瞻性研究显示,前述HCC风险评分均具有较高的预测准确度。应用这些评分工具可对患者进行风险分层,协助患者正确就医,甄别出最可能从治疗中获益的患者人群,从而在高发地区对医疗资源进行合理分配。
总 结
有效的抗病毒治疗虽不能完全阻止但可显著降低HCC发生,达到CHB治疗终点的关键在于药物选择。为了最大限度阻止终末期肝病尤其是HCC的发生,应对CHB患者给予有效且能快速降低病毒载量的药物治疗,并兼顾长期治疗的安全性以及低耐药发生率。ETV可强效持久抑制病毒复制,耐药发生率低,长期应用具有良好的安全性和耐受性,依从性好,可简化长期管理的难度,并被多项临床试验和临床实践数据证实,可有效减少HCC发生,是CHB患者最大化远期获益的优选药物之一。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#HCC#
45
#抗病毒#
43
#抗病毒治疗#
56
#APA#
45
#恩替卡韦#
33
#ASL#
44
#APASL#
44