Front Oncol:Lenvatinib(仑伐替尼)联合PD-1抑制剂一线治疗初始不可切除胆道癌(BTC)的疗效和安全性:单臂、开放标签II期临床研究
2021-11-27 yd2015 MedSci原创
研究表明,Lenvatinib联合PD-1抑制剂在初始不可切除的BTC患者中显示出了很好的抗肿瘤效果,并且耐受性良好。
胆道癌(BTC)是一组包括肝内胆管癌(ICC)、肝外胆管癌(ECC)和胆囊癌(GBC)的肿瘤,占原发性肝脏恶性肿瘤的10-15%。吉西他滨联合顺铂目前被推荐为晚期BTC患者的标准一线治疗。然而,该联合方案治疗相关的生存结果仍不是很好,中位总生存期(OS)约为6-8个月。因此,探索更有效的方案仍是必要的。近期,来自浙江大学医学院附属第二医院的团队开展了一项II期临床研究(ChiCTR2100044476),评估lenvatinib(仑伐替尼)联合程序性细胞死亡-1 (PD-1)抑制剂作为初始不可切除胆道癌(BTC)的一线治疗的疗效和安全性。相关结果发表在Frontiers in Oncology杂志上。

在这项II期临床研究中,初始无法切除BTC的患者接受lenvatinib(体重≥60 kg, 12 mg;<60kg, 8 mg)每日/次和PD-1抑制剂((pembrolizumab/ tislelizumab/sintilimab/camrelizumab 200 mg或toripalimab 240 mg)每3周/次。主要研究终点是客观缓解率(ORR)和安全性。次要终点包括手术转化率、疾病控制率(DCR)、无事件生存期(EFS)、总生存期(OS)和肿瘤生物标志物探索。
2018年3月1日至2021年5月31日,共纳入38例患者。在本分析的截止日期(2021年5月31日),共有23例(60.5%)患者停止治疗,15例(41.7%)仍在治疗。停止治疗最常见的原因是确认的进展性疾病或死亡(n=18)。3例患者接受二线联合化疗,2例因经济原因拒绝继续治疗。共有6例患者虽然证实肿瘤复发,但术后仍接受lenvatinib和抗pd -1抗体联合治疗。
5名(13.9%)患者和1名(2.8%)患者因TRAEs减少剂量和停止治疗。在研究期间,84.2%的患者经历了≥1次TRAE,没有治疗相关死亡。大多数TRAE低级别,易于管理。最常见的TRAE是疲劳(n=14),厌食症(n=8),谷丙转氨酶(ALT)升高(n=7)或天冬氨酸转氨酶(AST)升高(n=7),皮疹(n=6),高血压(n=5)和嗓音嘶哑(n=5)。34.2%的患者发生≥3级TRAE,最常见的是疲劳(n=5)和高血压(n=3)。
共有16例(42.1%,95% CI: 25.7% - 58.6%)患者获得了部分缓解,13例(34.2%,95% CI: 18.4% - 50.0%)病情稳定,没有患者获得完全缓解。ORR为42.1% (95% CI: 25.7% ~ 58.6%)。DCR为76.3 (95% CI: 62.2% ~ 90.5%)。

疗效评估
在38例可评估的患者中,34.2% (n=13)被认为适合切除。从开始全身治疗到手术的中位转化时间为5.5个月(95% CI: 3.8 - 7.1)。在接受转化手术的患者中,12例(92.3%)实现R0切除,1例由于腹部肿瘤远处转移而进行姑息性切除。在13例接受转换切除术的患者中,2例(15.4%)原发肿瘤实现MPR, 4例(30.8%)实现pPR。
中位随访时间为13.7个月(95% CI: 9.7 - 17.8), 1年OS率为47.4%(18/38),65.8%的患者仍然存活。中位EFS为8.0个月(95% CI: 4.6 - 11.4),中位OS为17.7个月(95% CI:不可估计)。在13例接受转化手术的患者中,中位EFS为13.5个月(95% CI: 13.0 - 14.0)。中位无复发生存(RFS)和中位OS未达到。在仅接受全身治疗的患者中,中位EFS为4.6个月(95% CI: 0.8 - 8.4),中位OS为12.4个月(95% CI: 8.5 - 16.3)。与仅接受全身治疗的患者相比,成功完成转化切除术的患者的EFS和OS更长。
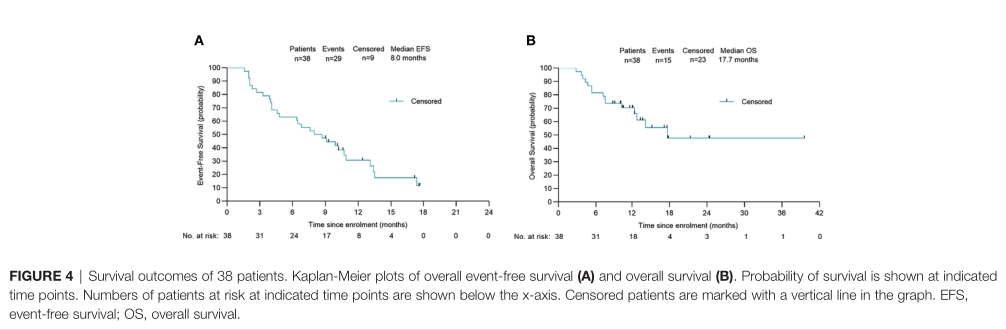
EFS和OS
在29例患者的预处理活检标本中评估PD-L1的表达。免疫组化显示,18例PD-L1阳性患者中有10例(61.1%)达到了客观反应(综合阳性评分[CPS]≥ 1%), 11例PD-L1阴性患者中有5例(45.5%)达到了客观反应。因此,PD-L1阳性表达患者的无事件生存(EFS) (P=0.009)和OS (P=0.013)均显著延长,提示PD-L1表达是一个潜在的预后因素。此外,在接受切除的患者亚组中,获得MPR或pPR的5例患者(80.0%)中有4例PD-L1阳性样本,而病理无反应的患者中只有57.1% PD-L1阳性。在免疫反应分析中,PD-L1表达阳性的患者肿瘤周围聚集的肿瘤浸润淋巴细胞较多。
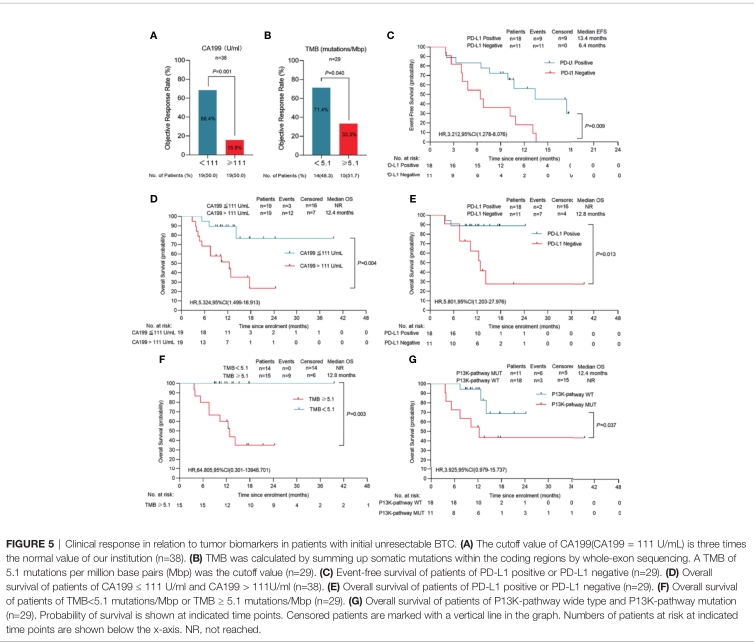
标志物探索
29例患者的中位TMB为5.10 muts/Mb。14例低TMB(中位数为5.10)患者中有10例(71.4%),15例高TMB患者中有5例(33.3%)达到了客观缓解。此外,低TMB患者的OS明显长于高TMB患者(P=0.003)。卡方分析表明,治疗前血清CA199水平与治疗效果相关。以111 U/mL为临界值,CA199水平低的患者与CA199水平高的组相比,ORR(68.4%)和OS延长(P=0.028)。在低CA199水平组,18例患者中有10例(55.6%)进行了切除,在数据截止时这些患者中没有发生死亡。有趣的是,与ECC或ICC患者相比,GBC患者有更高的ORR(61.5%)和更高的手术转化率(46.2%)。然而,由于样本量较小,在更大的GBC队列中进行进一步研究是有必要的。
综上,研究表明,Lenvatinib联合PD-1抑制剂在初始不可切除的BTC患者中显示出了很好的抗肿瘤效果,并且耐受性良好。
原始出处:
Zhang Q,Liu X, Wei S,Zhang L,Tian Y, Gao Z, Jin M and Yan S (2021) Lenvatinib Plus PD-1 Inhibitors as First-Line Treatment in Patients With Unresectable Biliary Tract Cancer: A Single-Arm, Open-Label, Phase II Study. Front. Oncol. 11:751391. doi: 10.3389/fonc.2021.751391
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#I期临床#
58
#抑制剂#
43
#疗效和安全性#
47
#II期临床研究#
44
胆道癌探索新治疗
55
#Oncol#
38
#PD-1抑制剂#
59
#lenvatinib#
47
#II期临床#
35
型肝炎的治疗方法因直接作用抗病毒
64