治疗C3肾小球肾炎,诺华的 iptacopan 在中期研究中达到临床终点
2021-11-15 Allan MedSci原创
C3G 的特点是过度活跃的替代补体途径,这反过来导致 C3 蛋白沉积物在肾小球中积聚。这会引发炎症和肾小球损伤,导致蛋白尿、血尿和肾功能下降。
致密沉积物病(dense deposit disease, DDD)和C3肾小球肾炎(C3 glomerulonephritis, C3G)是可累及儿童和年轻成人的罕见肾小球肾炎。这两种疾病都是由补体替代途径调节异常引起,现被归类为“C3肾小球病”。C3肾小球病较罕见,DDD的估计发病率为2-3例/100万人。大约 50% 的 C3G 患者在诊断后十年内进展为肾功能衰竭,并且在接受肾移植的患者中疾病复发并不少见。
C3G 的特点是过度活跃的替代补体途径,这反过来导致 C3 蛋白沉积物在肾小球中积聚。这会引发炎症和肾小球损伤,导致蛋白尿、血尿和肾功能下降。
诺华的研究性治疗药物 iptacopan(也称为 LNP023)在 II 期 C3 肾小球病 (C3G) 临床试验的两个患者队列中均达到了主要终点。在 II 期研究的最终分析中,患者每天两次接受 iptacopan 200mg,持续 12 周,并联合背景治疗。队列 A 包含患有 C3G 但未进行肾移植的患者——与基线相比,该队列中的患者蛋白尿减少了 45%。同时,队列 B 中的患者(包括肾移植后 C3G 恢复的患者)显示,与基线相比,C3 蛋白沉积物显著减少。
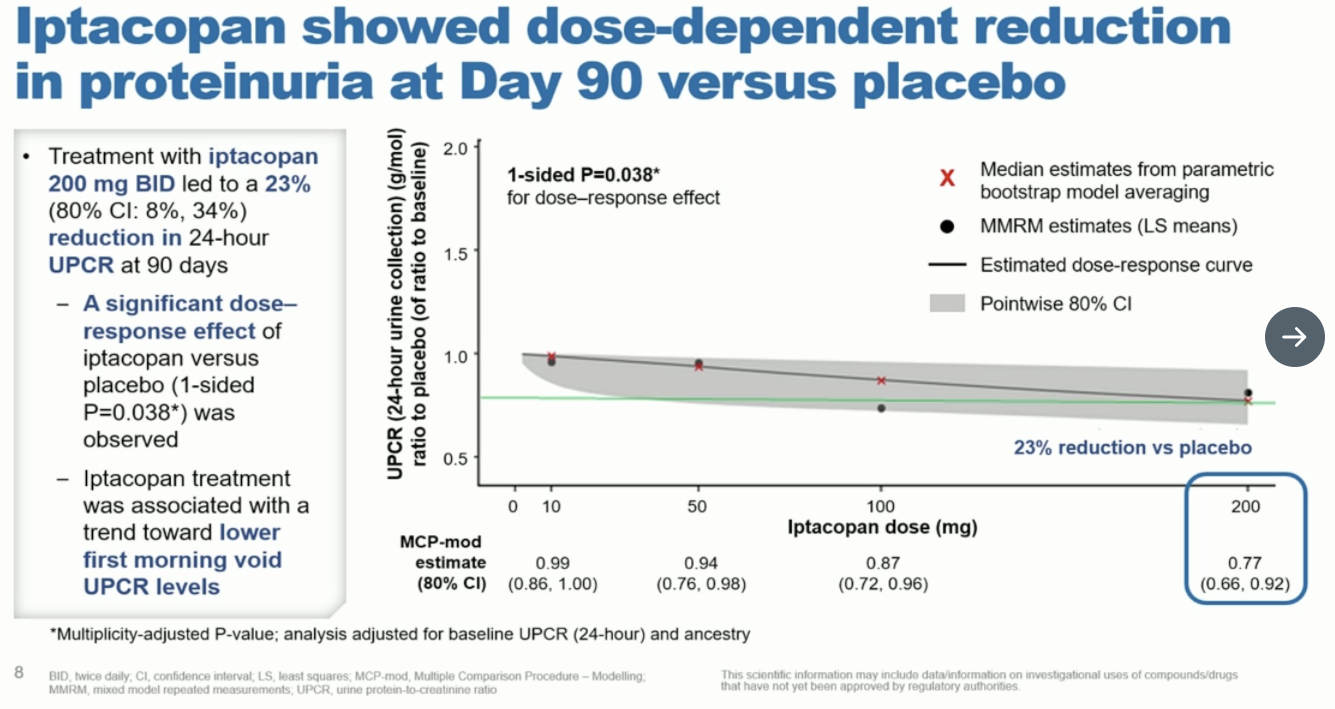
诺华补充说,这项研究中的两个队列都显示出对补体替代途径活性的强烈和持续抑制,以及 12 周内血清 C3 水平的正常化。
诺华全球药物开发负责人兼首席医疗官 John Tsai 说:“这些数据证明了 iptacopan 能够强烈而特异性地抑制 C3G 的关键驱动因素——替代补体途径。结果还显示了 iptacopan 为 C3G 患者提供首个靶向治疗的潜力,我们正在积极招募我们关键的 III 期 APPEAR-C3G 研究”。
原始出处:
https://www.pharmatimes.com/news/novartis_iptacopan_hits_endpoints_in_mid-stage_study_1383048
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#TAC#
36
#TACO#
40
#诺华#
50
#肾炎#
45
#肾小球肾炎#
44
通气患者的一个重要问题,其危险因
70