Cell:张锋发表综述详细介绍第二类CRISPR-Cas系统
2017-02-16 MedSci MedSci原创
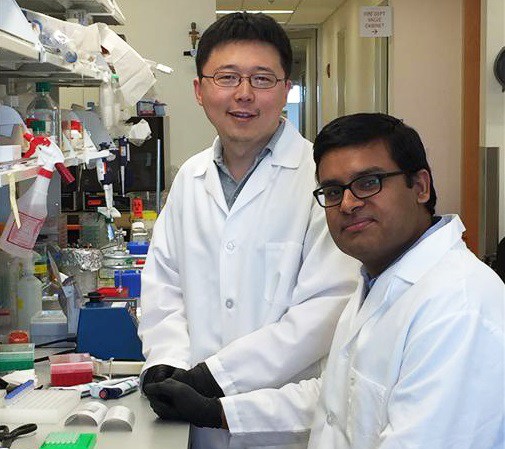
近期张锋教授也与另外两位学者在Cell杂志上发表了题为“SnapShot: Class 2 CRISPR-Cas Systems”的特写文章,介绍了新一代CRISPR基因组编辑系统:Class 2 CRISPR-Cas Systems。 2015年,张锋及其同事们就报告称发现了一种不同的CRISPR系统,具有潜力实现更简单、更精确的基因组工程操作。这个新系统是通过在不同类型的细菌中搜寻了成百上千
近期张锋教授也与另外两位学者在Cell杂志上发表了题为“SnapShot: Class 2 CRISPR-Cas Systems”的特写文章,介绍了新一代CRISPR基因组编辑系统:Class 2 CRISPR-Cas Systems。
2015年,张锋及其同事们就报告称发现了一种不同的CRISPR系统,具有潜力实现更简单、更精确的基因组工程操作。这个新系统是通过在不同类型的细菌中搜寻了成百上千种的CRISPR系统,寻找具有有用特性的酶,结果来自氨基酸球菌属(Acidaminococcus)和毛螺菌科(Lachnospiraceae)的Cpf1酶成为新的候选物。
这一新发现的Cpf1系统有几个重要的方面不同于以往描述的Cas9,在生物通最先报道的张锋Cell:新一代CRISPR基因组编辑系统这篇文章中就提到:Cpf1系统更简单一些,它只需要一条RNA。Cpf1酶也比标准SpCas9要小,使得它更易于传送至细胞和组织内;Cpf1以一种不同于Cas9的方式切割DNA。当Cas9复合物切割DNA时,它切割的是同一位点的两条链,留下的“平端”(blunt ends)在重新连接时往往会发生突变。采用Cpf1复合物生成的两条链切口是偏移的,在裸露端留下了短悬端(overhang)。这预计有助于精确插入,使得研究人员能够更有效及精确地整合一段DNA;Cpf1切口远离识别位点,这意味着即便在切割位点靶基因突变,仍然可以进行再度切割,提供了多次机会来校正编辑;Cpf1系统为选择靶位点提供了新的灵活性。像Cas9一样,Cpf1复合物必须首选附着PAM,短序列,选择的靶点靠近自然存在的PAM序列。Cpf1系统识别的PAM序列与Cas9截然不同。这在靶向某些基因组如疟原虫及人类基因组时可能是个优势。
这篇最新综述则更加概括的描述了这一系统,见下图:
文章指出,第二类CRISPR-Cas系统基于不同的效应蛋白家族,可以分为3种类型和9种亚型,其中譬如Cas9和Cas12a(Cpf1)已成功地用于基因组工程。在此前的研究中,张锋研究组也采用了一种新生物信息学方法来发现暂时被命名为C2c1、C2c2和C2c3的新蛋白,他们开发出一系列的计算方法来搜索NIH基因组数据库,鉴别新的CRISPR-Cas系统(详细见:Cell:第二代基因编辑神器诞生,CRISPR/Cpf1让一切皆有可能!)。
除此之外,张锋研究组也提出了一些新的尝试,如他们构建出了32个具有单个点突变的Cas9突变体,借助于已验证易错配的向导RNA将它们靶向EMX1基因。张锋将这些特异性增强型Cas9蛋白称作为“eSpCas9变体”。测试大量的向导RNAs与具单个点突变的eSpCas9和具三个点突变的eSpCas9,他们发现两种eSpCas9能够以相似的效率编辑靶位点。
张锋课题组还开发了一些基于功能获得性CRISPR的筛查方法。利用这一基于CRISPR的新工具来激活SAM基因,他的研究小组证实这一工具可以激活采用旧方法难于开启的12种不同的基因。“有许多基因采用旧系统无法激活,这一新系统能够激活转录达100倍或1000倍,”张锋说。
去年年底,张锋研究组发现Cpf1能够加工自己的CRISPR RNA (crRNA)。而且Cpf1介导的pre-crRNA加工是独立于DNA剪切的。这种能力可以用来简化多重基因组编辑。他们在此基础上设计CRISPR阵列,用一个载体同时在哺乳动物细胞编辑了四个基因,在小鼠大脑编辑了三个基因。这是在CRISPR–Cpf1的基础上打造了一个多重化基因编辑系统。
原始出处:
Makarova KS, Zhang F, Koonin EV. SnapShot: Class 2 CRISPR-Cas Systems. Cell. 2017 Jan 12;168(1-2):328-328.e1. doi: 10.1016/j.cell.2016.12.038.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#CEL#
32
#Cell#
30
#CRISPR#
29
#CRISPR-Cas#
40
#Cas#
24
好好努力
79
阅读了谢谢分享
81