Eur Heart J:非瓣膜性房颤患者持续服用口服抗凝药的预测因子、时间进程和结局
2021-07-19 MedSci原创 MedSci原创
至少四分之一的NVAF患者在4年内未持续使用OAC,这与缺血性卒中预防效果不佳有关。明确这类患者的基线特征可能有助于识别具有非持续性使用OAC风险的患者。
非瓣膜性心房颤动(NVAF)患者持续使用直接口服抗凝剂(DOAC)已成为一个问题,但很少研究这是否会影响患者预后。

近日,心血管领域权威杂志Eur Heart J上发表了一篇研究文章,研究人员调查了全国NVAF患者队列口服抗凝剂(OAC)持续性及其与预后之间的关联。
研究人员使用荷兰国家统计数据纳入了2013年至2018年期间开始使用以及未使用DOAC预防缺血性卒中的NVAF患者。根据最后一次处方和研究期结束之间100天的间隔来确定OAC的依从性。
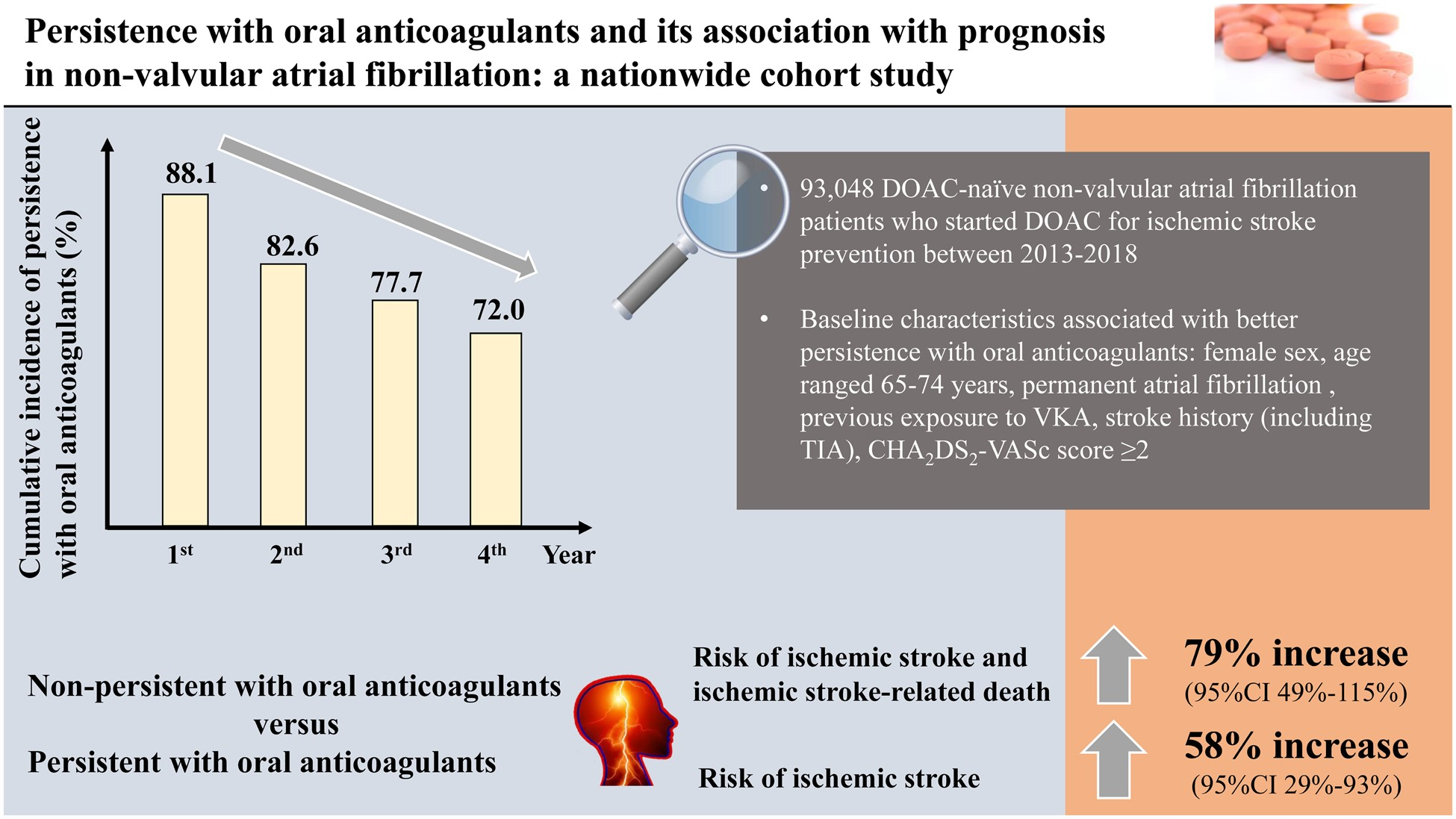
在93048名患者中,75.7%患者的基线CHA2DS2-VASc评分≥2。在接受DOAC后1、2、3和4年后持续服用OACs的累积发生率分别为88.1%[95%置信区间(CI)为87.9–88.3%]、82.6%(95%CI为82.3–82.9%)、77.7%(95%CI为77.3–78.1%)和72.0%(95%CI为71.5–72.5%)。与更好的OAC依从性相关的基线特征包括女性、年龄范围为65-74岁、永久性心房颤动、既往接触维生素K拮抗剂、卒中史(包括短暂性脑缺血发作)和CHA2DS2-VASc评分≥2。与持续使用OAC的患者相比,未坚持使用OAC与缺血性卒中和缺血性卒中相关死亡的复合结局[调整风险比(aHR)1.79,95%CI为1.49–2.15]和缺血性卒中(aHR1.58,95%CI1.29–1.93)。
由此可见,至少四分之一的NVAF患者在4年内未持续使用OAC,这与缺血性卒中预防效果不佳有关。明确这类患者的基线特征可能有助于识别具有非持续性使用OAC风险的患者。
原始出处:
Myrthe M A Toorop.et al.Predictors, time course, and outcomes of persistence patterns in oral anticoagulation for non-valvular atrial fibrillation: a Dutch Nationwide Cohort Study.European Heart Journal.2021.https://doi.org/10.1093/eurheartj/ehab421
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非瓣膜性房颤#
37
#瓣膜性#
48
#非瓣膜性#
53
#非瓣膜性房颤患者#
38
#预测因子#
38
#ART#
28
#口服抗凝药#
57
#HEART#
31
#瓣膜#
37
#房颤患者#
39