Movement Disorders:路易体病理和阿尔兹海默病理,如何影响男女的临床表型差异?
2022-05-29 网络 网络
使用LB和AD生物标志物,即使在LB或AD病理不在临床预期之内,对于LB疾病和AD的准确临床诊断也是必要的。
继阿尔茨海默病(AD)之后,路易体(LB)疾病是第二种最常见的神经退行性痴呆疾病,包括帕金森病、帕金森病痴呆和路易体痴呆。这些疾病有一系列重叠的临床特征、遗传风险因素,以及α-突触核蛋白阳性的路易体和路易体神经元的共同神经病理学特征。
图1: 论文封面图
目前,神经病理学确认仍然是诊断LB病的金标准,而对有LBs的痴呆和早期帕金森病的临床诊断准确率仍然只有50%左右,这大大限制了将早期患者分配到疾病改良剂临床试验中的努力。 在那些同时患有LB和AD病症的患者中,较高的神经纤维缠结负担与较低的LB痴呆临床诊断的可能性有关,这可能是因为相关的认知特征的改变和较低的LB核心特征如视幻觉的可能性。
性别也与纯LB病理者的表型差异以及LB病理者的AD共病理的频率有关。与男性相比,混合LB和AD病理在女性中更常见,而纯LB病理不太可能导致LB临床表型,在女性中更可能出现AD临床表型。在AD中,女性比男性有更大的tau负担,有类似的认知障碍,而且女性在发展认知衰退之前可以承受更多的tau。 然而,在有LB病理的人中,性别和AD共病理学,特别是tau的交互影响仍然未知。
藉此,加州大学圣地亚哥的Ece Bayram等人,利用国家阿尔茨海默氏症协调中心(NACC)收集的大规模、多中心的尸检验证个体数据,分析了AD共病理学和LB疾病核心临床特征之间的性别差异,包括认知波动、视觉幻觉、快速眼动睡眠行为障碍(RBD)和帕金森症。
还评估了性别特异性Braak tau分期与临床特征的关系。由于LB痴呆症患病率的性别差异可能取决于年龄,70-75岁以下的男性患病率较高,女性患病率随年龄增长而增加,通过对年龄分层组的额外分析调查了年龄的影响。
核心假设,那些有更多AD病理的人将不太可能有LB临床表型,而且与男性相比,女性对LB病理患者的误诊率会更高。
该研究的数据来自国家阿尔茨海默病协调中心,有223名女性和468名男性肢体或新皮层LB患者,根据病理学分为两组,即LB临床表型的高可能性和低/中可能性。分析了性别的临床关联以及性别和病理学对临床表型的交互作用。
他们发现:更严重的AD共病理学与更差的认知衰退和较低的LB疾病临床表型的可能性有关。
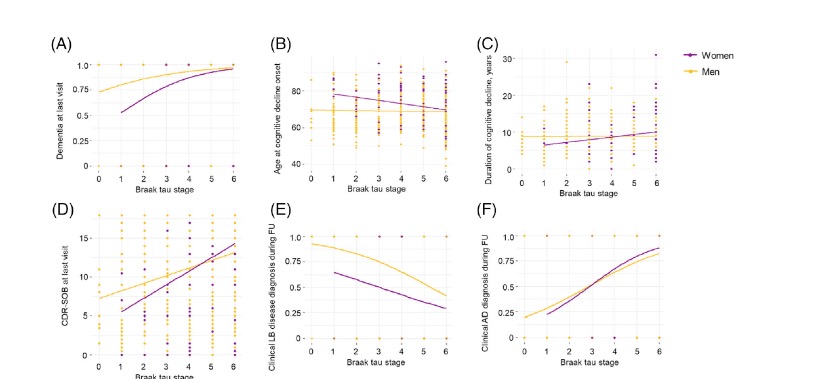
图2:论文结果图
与男性相比,具有更严重的AD共病理学和tau的女性有更差的认知衰退和更高的AD临床表型的可能性。
与女性相比,具有更严重的AD共病理学的男性具有较低的LB临床表型的可能性。性别和病理的相互作用在70-80岁之间的人中更为明显。
AD共病理学降低了女性和男性出现LB临床表型的可能性;然而,男性可能有较高的LB疾病诊断不足的风险,女性则有较高的痴呆风险。使用LB和AD生物标志物,即使在LB或AD病理不在临床预期之内,对于LB疾病和AD的准确临床诊断也是必要的。
原文出处:
Bayram E, Coughlin DG, Litvan I. Sex Differences for Clinical Correlates of Alzheimer’s Pathology in People with Lewy Body Pathology. Movement Disorders. Published online May 9, 2022:mds.29044. doi:10.1002/mds.29044
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


















#Disord#
73
#ERS#
37
#路易体#
50
#Dis#
47
#disorder#
50
#disorders#
37
#阿尔兹海默#
51
#临床表型#
50
#表型#
46