Hypertension:白细胞介素-1β抑制对血压、高血压发病率和炎症风险的影响
2020-12-10 MedSci原创 MedSci原创
虽然高血压与炎症相关,但专门针对炎症的疗法对血压的影响尚不确定。最近的CANTOS探究了IL(白细胞介素)-1β抑制是否会降低血压、预防高血压事件,以及改变高血压和心血管事件之间的关系。
虽然高血压与炎症相关,但专门针对炎症的疗法对血压的影响尚不确定。最近的CANTOS探究了IL(白细胞介素)-1β抑制是否会降低血压、预防高血压事件,以及改变高血压和心血管事件之间的关系。
研究纳入10061名既往有心肌梗死且hsCRP(高敏C反应蛋白)≥2 mg/L的患者,随机分配到卡那金单抗50 mg、150 mg、300 mg或安慰剂组。共有9549名试验参与者在随访期间记录了血压;其中,80%的试验参与者已诊断为高血压。
结果显示,在没有基线高血压的患者中,hsCRP基线分位数最低到最高的患者,每100人年的高血压事件发生率分别为23.4、26.6和28.1(P>0.2)。在所有参与者中,接受卡那金单抗并不能降低受试者随访期间的血压(P>0.2)或事件性高血压(HR,0.96[0.85-1.08],P>0.2)。IL-1β抑制与卡那金单抗可降低主要不良心血管事件发生率。
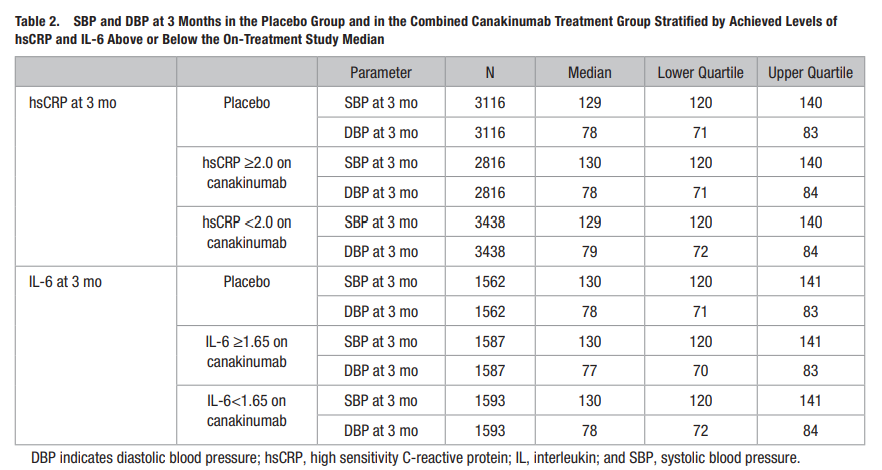
这些分析表明,这种益处的机制与血压或高血压事件的变化无关。
原始出处:
Alexander Mk Rothman, Jean MacFadyen, et al., Effects of Interleukin-1β Inhibition on Blood Pressure, Incident Hypertension, and Residual Inflammatory Risk: A Secondary Analysis of CANTOS. Hypertension. 2020 Feb;75(2):477-482. doi: 10.1161/HYPERTENSIONAHA.119.13642.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#发病率#
25
#白细胞介素-1β#
34
#PE#
25
#Hypertension#
35
#白细胞介素#
35
#TENS#
24
可能确实没啥太大的关系。
0
学习了
66