Cell Rep:科学家找到靶向KRAS途径治疗肺癌的新靶点
2016-08-02 佚名 生物谷
美国西南医学中心的研究人员最近发现了一条通过靶向KRAS基因治疗肺癌的新途径。KRAS基因是人类癌症中最常见的突变基因之一,也是很难成功进行靶向治疗的一个基因。 之前研究表明KRAS基因的编码产物K-Ras会影响细胞分裂,因此KRAS基因发生突变会导致正常细胞出现增殖失控从而发生癌变。 突变的KRAS不仅能够促进肿瘤生长,还会帮助肺癌细胞存活。但是目前仍然没有抑制突变KRAS的有效的临床用

美国西南医学中心的研究人员最近发现了一条通过靶向KRAS基因治疗肺癌的新途径。KRAS基因是人类癌症中最常见的突变基因之一,也是很难成功进行靶向治疗的一个基因。
之前研究表明KRAS基因的编码产物K-Ras会影响细胞分裂,因此KRAS基因发生突变会导致正常细胞出现增殖失控从而发生癌变。
突变的KRAS不仅能够促进肿瘤生长,还会帮助肺癌细胞存活。但是目前仍然没有抑制突变KRAS的有效的临床用药,因此开发有效的临床靶向治疗药物得到了许多研究的关注。
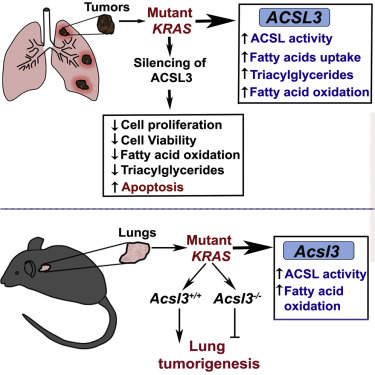
在该研究中研究人员对肺癌中的KRAS进行了研究,发现ACSL3介导的KRAS活性对于肺癌细胞存活至关重要,抑制ACSL3就会引起肺癌细胞死亡。
研究人员发现ACSL3的酶活性是突变的KRAS基因促进肺癌形成所需要的一个重要条件,进一步研究表明ACSL3的催化底物——脂肪酸在肺癌中扮演重要角色。
研究人员表示:“这些结果非常重要。大约30%的肺癌病例中都存在KRAS基因突变,并且KRAS基因突变还与癌症的侵袭性以及治疗抵抗都存在相关性,除此之外携带突变的病人其预后也很差。根据美国国家癌症研究所的统计数据,肺癌仍然是美国癌症相关死亡的头号原因。”
“目前急需发现更多靶点来抑制癌细胞的脂质代谢,从而开发靶向治疗方法,而该研究发现ACSL3在肺癌中的重要性恰好填补了这一需求。”文章第一作者Dr. Mahesh S. Padanad这样说道。
该研究发表在国际学术期刊Cell Reports上。
原始出处
Mahesh S. Padanad1, 2, 12, Georgia Konstantinidou1, 2, 12, 13, Niranjan Venkateswaran1, 2, Margherita Melegari2, Smita Rindhe1, 2, Matthew Mitsche3, 4, Chendong Yang5, Kimberly Batten6, Kenneth E. Huffman7, Jingwen Liu8, Ximing Tang9, Jaime Rodriguez-Canales9, Neda Kalhor9, Jerry W. Shay6, John D. Minna1, 7, Jeffrey McDonald4, Ignacio I. Wistuba10, 11, Ralph J. DeBerardinis3, 5, Pier Paolo Scaglioni.Fatty Acid Oxidation Mediated by Acyl-CoA Synthetase Long Chain 3 Is Required for Mutant KRAS Lung Tumorigenesis.Cell Rep.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Cell#
26
#CEL#
24
值得关注
97
#新靶点#
35
#KRAS#
32
好好学习
83