HAEMATOLOGICA:过氧化物酶体增殖物激活受体 α 在高脂血症下促进血小板高反应性和血栓形成中的关键作用
2021-10-09 MedSci原创 MedSci原创
血小板ppar α 会严重介导血小板活化,并有助于高脂血症下的血栓形成状态
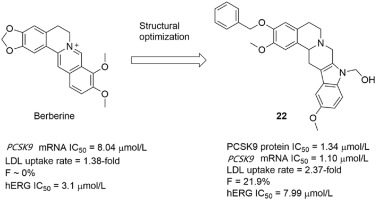
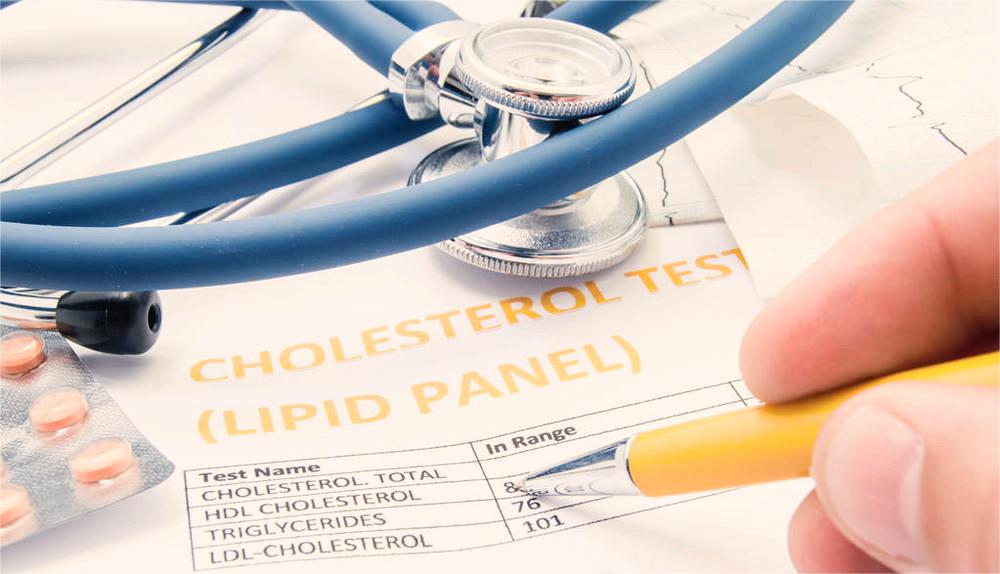
基于血小板过度活跃的动脉粥样硬化血栓性疾病是世界范围内死亡和发病率的主要原因。血小板高反应性和动脉粥样硬化血栓形成风险增加与血脂异常特别相关。过氧化物酶体增殖物激活受体 α (ppar α) 是脂质代谢的重要调节剂。尽管人们积极努力建立血脂异常中导致血小板过度活跃的通路,但其相关机制仍不清楚。识别血脂异常调节血小板活性的关键靶点对于预防和管理动脉粥样硬化血栓性疾病至关重要。

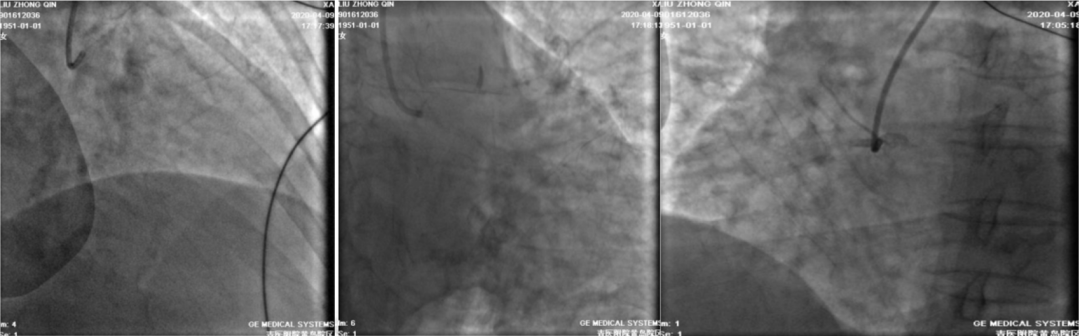
在这项研究中,研究了ppar α 在与血脂异常相关的血小板活化和血栓形成中的作用及其机制。使用缺失ppar α (ppar α -/-) 的小鼠,研究团队证明ppar α 是血小板活化和血栓形成所必需的。Ppar α 的作用主要取决于血小板致密颗粒的分泌,并由p38MAPK/Akt,脂肪酸 β-氧化和NAD(P)H氧化酶 (NOX) 途径引起。重要的是,ppar α 和相关途径介导了高脂饮食 (HFD) 诱导的血栓前状态和氧化的低密度脂蛋白 (oxLDL) 引起的血小板过度活跃。野生型 (WT),嵌合 (ppar α/-) 和ppar α -/-小鼠的数据显示,血小板反应性与ppar α 的表达水平呈正相关。这种正相关关系在高脂血症患者的血小板中得到概括。在脂质处理的巨核细胞系中,脂质诱导的活性氧 (ROS)-NF-κ b途径被发现在高脂血症中上调血小板ppar α。这些数据表明,血小板ppar α 会严重介导血小板活化,并有助于高脂血症下的血栓形成状态。
综上所述,他们发现血小板PPARα通过促进颗粒密集分泌,正向介导血小板活化。高脂血症可能通过上调巨核细胞/血小板中PPARα的表达和PPARα在血小板中介导的激活信号的增强来促进血栓前状态。这项工作表明,针对PPARα的基因组和非基因组联合干预可能对预防高脂血症下的血栓形成是必要的。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#反应性#
52
#血小板高反应性#
52
#HAE#
30
#中的关键作用#
36
#EMA#
39
#高脂#
32