高脂血症的常用药物,一网打尽!
2021-08-30 MedSci原创 MedSci原创
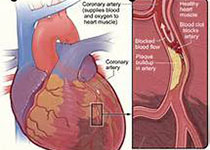
血脂和脂蛋白代谢乱与动脉粥样硬化密切相关,血脂异常的治疗目的在于降低缺血性心血管疾病(冠心病和缺血性脑卒中)的患病率和死亡率。
血脂和脂蛋白代谢乱与动脉粥样硬化密切相关,血脂异常的治疗目的在于降低缺血性心血管疾病(冠心病和缺血性脑卒中)的患病率和死亡率。许多研究证实,降低血浆胆固醇能减少冠心病的发病率及死亡率,血浆胆固醇降低1%,冠心病事件发生的危险性可降低2%。目前认为胆固醇(TC)、低密度脂蛋白胆固醇(LDL-C)、甘油三酯(TG)和极低密度脂蛋白(VLDL)增高是冠心病的危险因素,其中LDL-C最为重要,而HDL-C则被认为是冠心病的保护因素。对于继发性血脂异常应以治疗原发病为主,如糖尿病、甲状腺功能减退症经过控制后,血脂有可能恢复正常。但是原发性和继发性血脂异常可能同时存在,如果原发病经过治疗正常一段时间后,血脂异常仍然存在,考虑同时伴有原发性血脂异常,需给予相应治疗。
目前以综合治疗为主,其中生活方式干预是首要的基本治疗措施,药物治疗易接受且效果肯定,注意严格掌握指征,血浆净化疗法或外科治疗是药物治疗的补充,基因治疗尚在探索之中。本文带领大家一起了解一下临床常用的降脂药物。
一、HMG-CoA还原酶抑制剂(他汀类)
1.主要适应症:LDL-C升高,心血管风险升高
2.机制:降低胆固醇合成,增加肝LDL-C受体,减少VLDL生成
3.常见副作用:肌痛、关节痛、转氨酶升高、消化不良
4.代表药物:
|
代表药物 |
起始剂量 |
最大剂量 |
|
洛伐他汀 |
20-40mg,qd |
80mg,qd |
|
普伐他汀 |
40-80mg,qd |
80mg,qd |
|
辛伐他汀 |
20-40mg,qd |
80mg,qd |
|
氟伐他汀 |
20-40mg,qd |
80mg,qd |
|
阿托伐他汀 |
20-40mg,qd |
80mg,qd |
|
瑞舒伐他汀 |
5-20mg,qd |
40mg,qd |
|
匹伐他汀 |
1-2mg,qd |
4mg,qd |
注:qd,每日一次
二、胆固醇吸收抑制剂
1.主要适应症:LDL-C升高
2.机制:降低胆固醇合成,增加肝LDL-C受体
3.常见副作用:转氨酶升高
4.代表药物:依折麦布,起始剂量:10mg,qd,最大剂量:10mg,qd。
三、胆汁酸螯合剂
1.主要适应症:LDL-C升高
2.机制:增强胆汁酸排泄,增加肝LDL-C受体
3.常见副作用:腹胀、便秘、甘油三酯升高
4.代表药物:
|
代表药物 |
起始剂量 |
最大剂量 |
|
考来烯胺 |
4g,qd |
32g,qd |
|
考来替泊 |
5g,qd |
40g,qd |
|
考来维仑 |
3750mg,qd |
4375mg,qd |
注:qd,每日一次
四、MPT抑制剂
1.主要适应症:纯合型家族性高胆固醇血症(HoFH)
2.机制:减少VLDL合成
3.常见副作用:皮肤潮红、腹泻、增加肝脏脂肪
4.代表药物:洛美他派甲磺酸盐,起始剂量:5mg,qd,最大剂量:60mg,qd。
五、ApoB抑制剂
1.主要适应症:纯合型家族性高胆固醇血症(HoFH)
2.机制:减少VLDL合成
3.常见副作用:注射部位反映、流感样症状、增加肝脏脂肪
4.代表药物:米泊美生,起始剂量:200mg,皮下注射(SC),qw,最大剂量:200mg,SC,qw。
六、烟酸
1.主要适应症:LDL-C升高,TG升高
2.机制:减少VLDL合成
3.常见副作用:皮肤潮红、胃肠道不适、血糖升高、血尿酸升高、肝功能受损
4.代表药物:
|
代表药物 |
起始剂量 |
最大剂量 |
|
快速释放型 |
100mg,tid |
1g,tid |
|
持续释放型 |
250mg,bid |
1.5g,bid |
|
延长释放型 |
500mg,qn |
2g,qn |
注:tid,每日三次,bid,每日两次,qn,睡前
七、纤维酸衍生物
1.主要适应症:TG升高
2.机制:减少VLDL合成,增加脂蛋白脂肪酶水平
3.常见副作用:消化不良、肌痛、胆结石、转氨酶升高
4.代表药物:
|
代表药物 |
起始剂量 |
最大剂量 |
|
吉非贝齐 |
600mg,bid |
600mg,bid |
|
非诺贝特 |
145mg,qd |
145mg,qd |
注:qd,每日一次,bid,每日两次
八、ω-3脂肪酸
1.主要适应症:TG升高
2.机制:增加TG分解代谢
3.常见副作用:消化不良、鱼腥味呼吸气味
4.代表药物:
|
代表药物 |
起始剂量 |
最大剂量 |
|
ω-3酸乙酯 |
4g,qd |
4g,qd |
|
二十碳五烯酸乙酯 |
4g,qd |
4g,qd |
注:qd,每日一次
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












全
42
#高脂血症##科普#
90
#常用药物#
50
这个很好,很全面,
50
#高脂#
41
#常用药#
31