先天性双主动脉弓血管环患儿气管异物麻醉处理1例
2018-10-15 王建设 费建 赵龙德 中国内镜杂志
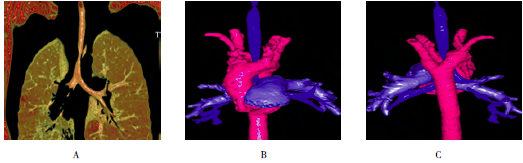
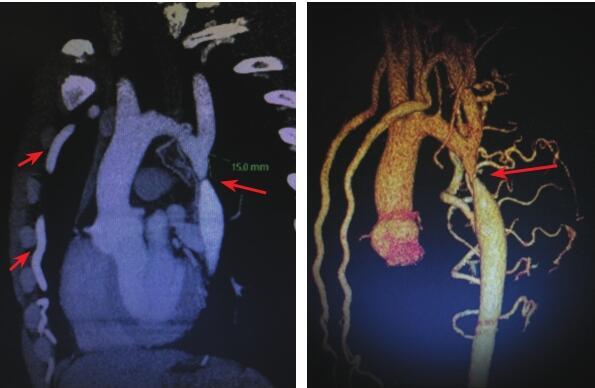
患儿女,8岁3个月,20kg,因“咳嗽2个月余”于2016年5月9日入院,期间外院抗感染治疗效果欠佳,反复发作咳嗽、气喘。该院胸部CT考虑“支气管异物,双主动脉弓”(图1)。平素挑食,否认既往呼吸及吞咽困难病史。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#血管环#
29
#麻醉处理#
45
#先天性#
41
#主动脉#
45
#主动脉弓#
42