肺栓塞诊断的11种方法
2016-07-20 张明明 医学界呼吸频道
急性肺栓塞是静脉血栓栓塞症中最为严重的临床表现,常无明显症状,临床偶然发现后确诊,而部分患者由于发病急骤、病情危重,首发表现为猝死。根据病人VTE易患因素,对可疑患者进行相关辅助检查。那么相关的辅助检查有哪些呢?1.动脉血气分析检查时患者取卧位、未吸氧状态的首次动脉血气分析为准,其动脉血气可表现为低氧血症、低碳酸血症、肺泡-动脉血氧梯度增大及呼吸性碱中毒,但还有一部分患者血氧饱和度正常。此项检查无
急性肺栓塞是静脉血栓栓塞症中最为严重的临床表现,常无明显症状,临床偶然发现后确诊,而部分患者由于发病急骤、病情危重,首发表现为猝死。根据病人VTE易患因素,对可疑患者进行相关辅助检查。那么相关的辅助检查有哪些呢?
1.动脉血气分析
检查时患者取卧位、未吸氧状态的首次动脉血气分析为准,其动脉血气可表现为低氧血症、低碳酸血症、肺泡-动脉血氧梯度增大及呼吸性碱中毒,但还有一部分患者血氧饱和度正常。此项检查无特异性。
2.血浆D-二聚体
血浆D-二聚体升高的阳性预测价值较低,除了急性血栓形成时,还可见于肿瘤、炎症、出血、外伤、外科手术等,但其阴性预测价值很高,正常水平可排除急性肺栓塞。推荐使用定量酶联免疫吸附试验(ELISA)或其衍生法来对门诊和急诊疑似急性肺栓塞患者进行检测,为高度检测法,敏感度>95%。但其结果主要用于排除急性肺栓塞,而非确诊。对于老年患者,其血浆D-二聚体检测特异性随年龄增加而降低,建议对老年患者血浆D-二聚体水平的评估进行校正,以年龄校正临界值,增加其特异度。
3.心电图
常表现为胸前导联V1-V4及肢体导联II、III、aVF的ST段压低和T波倒置,V1为QR型,SIQIIITIII(即I导联S波加深、III导联出现Q/q波及T波倒置),不完全性或完全性右束支传导阻滞。轻者可仅表现为窦性心动过速。可出现房性心律失常,常见为房颤。
4.超声心动图
肺栓塞的直接征象为发现肺动脉近端或右心腔血栓;间接征象为右心负荷过重,如右心室壁局部运动幅度下降,右心室和(或)右心房扩大,三尖瓣反流速度增快以及室间隔左移,肺动脉干增宽等。对于提示诊断、预后评估及除外其他心血管疾病有重要价值。
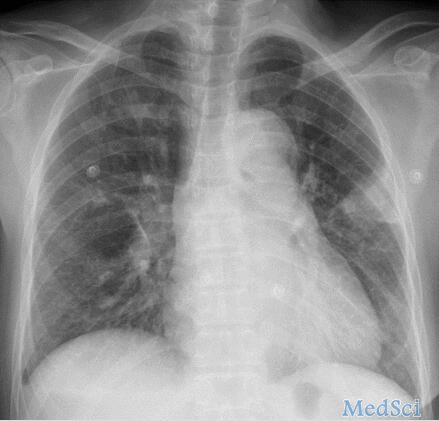
5.胸部X线平片
急性肺栓塞若引发肺动脉高压或肺梗死,X线平片可见肺纹理稀疏、纤细的肺缺血征象,肺动脉段突出或瘤样扩张,肺动脉干增宽或伴截断征,右心室扩大征。也可出现肺野局部浸润阴影、尖端指向肺门的楔形阴影、盘状肺不张、患侧膈肌抬高、肋膈角变钝、胸膜增厚粘连等。可协助排除其他原因导致的呼吸困难和胸痛。
6.CT肺动脉造影
此为直观判断肺动脉栓塞程度和形态、累及部位及范围的无创检查。急性肺栓塞的直接征象为肺动脉内低密度充盈缺损,部分或完全包围在不透光的血流之内的“双轨征”,或者呈完全充盈缺损,远端血管不显影。间接征象有肺野楔形条带状高密度区或盘状肺不张,中心肺动脉扩张及远端血管分布减少或消失等。
但其对亚段及以下的肺动脉血栓敏感度较差,故其阴性结果不能排除单发的亚段栓塞,需进一步结合下肢静脉超声、肺通气灌注扫描或肺动脉造影等检查明确诊断。
7.放射性核素肺通气灌注扫描
典型征象为与通气显像不匹配的肺段分布灌注缺损,其敏感度和特异度均较高(92%和87%),且不受肺动脉直径的影响,尤其在诊断亚段以下急性肺栓塞的诊断中具有特殊意义。但应排除其他引发肺部血流或通气受损的因素,如肺部炎症、肿瘤等,部分患有基础心肺疾病的患者也不耐受此项检查。
8.磁共振肺动脉造影(MRPA)
在单次屏气20秒内完成MRPA扫描,可确保肺动脉内较高信号强度,直接显示肺动脉内栓子及急性肺栓塞所致的低灌注区。优势在于可以同时评估患者右心功能,对于无法进行造影的碘过敏患者也适用。缺点在于同样不能作为独立排除急性肺栓塞的检查。
9.肺动脉造影
急性肺动脉栓塞的“金标准”,直接征象为肺动脉造影剂充盈缺损,伴或不伴“轨道征”的血流阻断;间接征象有肺动脉造影剂流动缓慢,局部低灌注,静脉回流延迟。对于排除了ACS的血流动力学不稳定者,可考虑肺动脉造影,必要时可同时行经皮导管介入治疗。
10.下肢深静脉检查
DVT与急性肺栓塞形成有密切关系,对下肢静脉行超声检查可为急性肺栓塞的诊断提供依据。
11.遗传性易栓症相关检查
建议对以下情况患者进行遗传性易栓症筛查:
(1)发病年龄较轻(<50岁);
(2)有明确的VTE家族史;
(3)复发性VTE;
(4)少见部位(如下腔静脉,肠系膜静脉;脑、肝、肾静脉等)的VTE;(5)无诱因VTE;
(6)女性口服避孕药或绝经后接受雌激素替代治疗的VTE;
(7)复发性不良妊娠(流产,胎儿发育停滞,死胎等);
(8)口服华法林抗凝治疗中发生双香豆素性皮肤坏死;
(9)新生儿暴发性紫癜。
中国人最常见的遗传性易栓症是抗凝蛋白缺陷,建议筛查抗凝血酶、蛋白C和蛋白S的活性,对于活性下降者有条件应进行相关抗原水平测定以明确抗凝蛋白缺陷的类型。对于哈萨克、维吾尔等高加索血统的少数民族除了筛查上述项目外,还应检测凝血因子V Leiden突变和PTG20210A突变。上述检测未发现缺陷的VTE患者,建议进一步检测血浆同型半胱氨酸(MTHFR突变),血浆因子VIII、IX、XI和纤溶蛋白等。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












文章很好值得关注
68
不错哦继续关注
69
一堆检查而已
36
越来越多
78
关注le
84
值得收藏
38