J Gastrointest Surg:啥?术前检测CEA水平可提高结肠癌的风险分层?
2017-07-09 guojiangui 肿瘤资讯
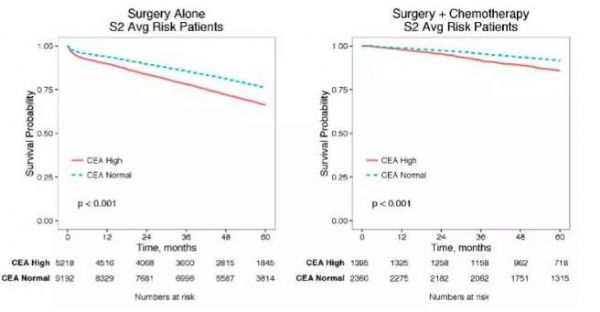
今年5月,一项由梅奥诊所研究人员发表在胃肠外科杂志(Journal of Gastrointestinal Surgery)的研究表示,术前检测血清中癌胚抗原(CEA)的水平,可以提高Ⅱ期结肠癌患者的术前风险分层和指导选择辅助化疗方案。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#EST#
32
#AST#
35
#GAS#
32
#Test#
33
#风险分层#
28
#CEA#
25
学习
50
病毒血液截留吸附术
53
学习,谢谢分享
46
学习了,涨知识
48