“神药”成癌症免疫治疗理想拍档?他汀类或为抗PD-1单药治疗的非小细胞肺癌患者带来生存获益!
2022-05-11 LILYMED MedSci原创
BMC cancer:他汀类药物治疗对接受抗PD-1单药治疗的非小细胞肺癌患者结局影响的倾向评分匹配分析:一项多中心回顾性研究
靶向程序性细胞死亡-1 (PD-1)/程序性细胞死亡-配体 1 (PD-L1) 途径的免疫检查点抑制剂 (ICI) 是癌症患者的标准治疗选择。然而,许多先前的报告显示,少数非小细胞肺癌(NSCLC)患者在临床环境中对ICIs有反应。因此,我们需要确定提高癌症免疫疗法疗效的策略。最近,许多研究描述了与接受癌症免疫治疗的NSCLC患者的反应和生存相关的伴随药物,包括抗生素,质子泵抑制剂,益生菌,β受体阻滞剂和二甲双胍,因此可能还有其他药物可以改善接受癌症免疫治疗的NSCLC患者的预后。
他汀类药物是被广泛处方的降胆固醇药物,通过抑制甲羟戊酸途径的限速酶(支持肿瘤发生并在癌症中不受调节)来抑制3-羟基-3-甲基戊二酰辅酶A(HMG-CoA)向甲羟戊酸的转化。许多回顾性研究表明,他汀类药物的使用与癌症风险和复发或癌症特异性死亡率的降低有关。此外,根据之前的报告,他汀类药物也有望改善癌症免疫治疗的效果。因此,本研究探索了他汀类药物治疗对抗PD-1单药治疗的NSCLC患者生存率的临床影响。这项多中心和回顾性研究进行了倾向评分匹配分析,以尽量减少患者背景产生的偏倚。

原始队列中的患者特征
表1显示了参加本研究的390名患者的临床特征。中位年龄为67岁(范围,31 -88岁),309名(79.2%)患者为男性。在390例患者中,53例(13.6%)接受他汀类药物治疗,包括阿托伐他汀12例,匹伐他汀10例,普伐他汀9例,瑞舒伐他汀19例,辛伐他汀3例。326名患者(83.6%)有EGFR或ALK状态数据,261名患者(66.9%)有PD-L1数据。
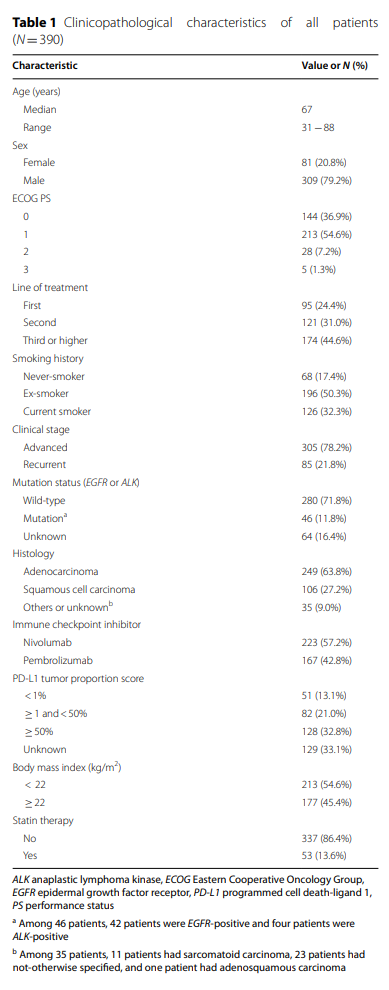
表2根据他汀类药物治疗总结患者的基线特征,他汀类药物的使用或不使用与原始队列中的年龄,性别,吸烟史,BMI和突变状态相关(P<0.0001,P = 0.0036,P = 0.0085,P = 0.0032和P = 0.0508)。

原始队列的生存分析结果
首先研究他汀类药物治疗对原始队列中生存的影响。中位随访时间为416天(范围,3-1701)。在这项研究中,没有患者死于肺癌以外的任何疾病。Kaplan-Meier曲线显示,接受和未接受他汀类药物治疗的患者之间的PFS或OS没有显著差异(P = 0.4777和P = 0.5264)。多变量分析显示,ECOG PS(PS 1 − 3 vs. PS 0: HR = 1.36,P = 0.0084)、吸烟史(从不吸烟者与吸烟者:HR = 1.37,P = 0.0298)和PD-L1表达状态(其他与≥TPS 50%:HR = 1.64,P < 0.0001)是PFS的独立预后因素,而ECOG PS(PS 1 − 3 vs. PS 0: HR = 1.66,P = 0.0001)和PD-L1表达状态(其他与≥TPS 50%:HR = 1.52,P = 0.0026)是OS的独立预后因素。
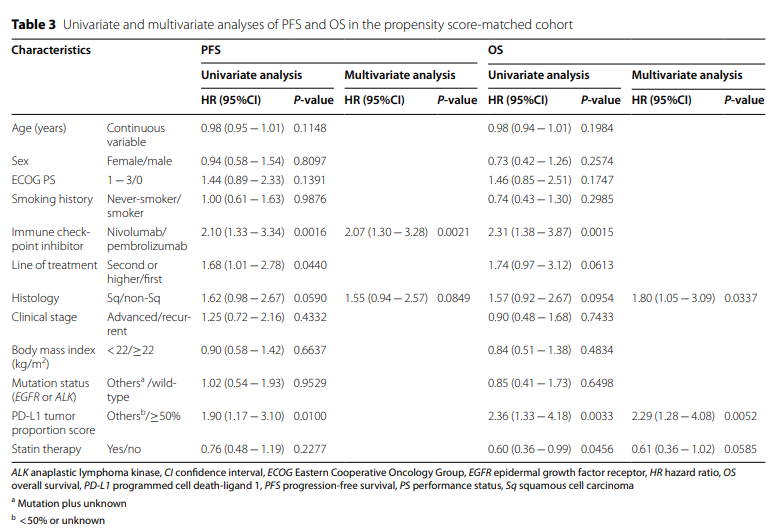
倾向评分匹配队列的生存分析结果
接下来研究他汀类药物治疗对倾向评分匹配队列中生存率的影响。中位随访时间为457天(范围,15-1358)。Kaplan-Meier曲线显示,相比没有接受他汀类药物治疗的患者,接受他汀类药物治疗患者的OS明显更长(P = 0.0433),但不包括PFS(P = 0.2251)(图2)。Cox分析显示,ICI的使用是PFS的独立预后因素(nivolumab vs. pembrolizumab:HR = 2.07,P = 0.0021;表3),而组织学(Sq vs. non-Sq: HR = 1.80, P = 0.0337)和PD-L1表达状态(其他与≥ TPS 50%: HR = 2.29, P = 0.0052)是OS的独立预后因素。倾向评分匹配队列中的Cox回归分析显示,他汀类药物治疗的使用不是一个独立的有利预后因素,尽管它往往与有利的结局相关(使用与不使用:HR = 0.61,P = 0.0585)。
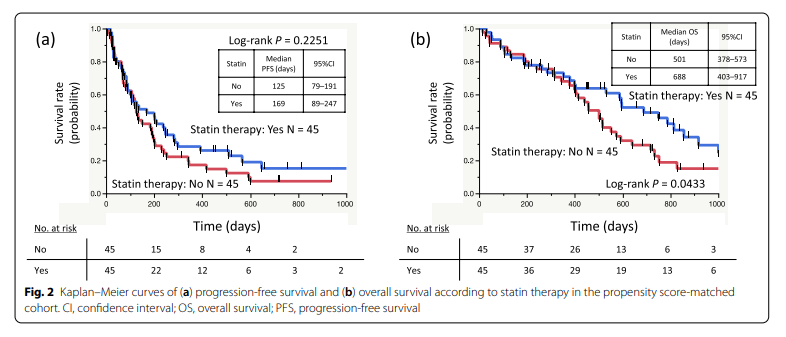
在这项多中心和回顾性研究中,在原始队列中,使用和不使用他汀类药物治疗的NSCLC患者之间未观察到PFS和OS的显著差异。然而,接受他汀类药物治疗的NSCLC患者的患者特征与年龄、性别、吸烟史、BMI和突变状态相关,研究结果与先前报道的结果相似。在通过倾向评分匹配调整这些偏倚后,接受他汀类药物治疗的NSCLC患者的OS比未接受他汀类药物治疗的患者具有显着更长的OS。因此,本研究结果表明,使用他汀类药物可能有助于接受抗PD-1单药治疗的NSCLC患者的有利预后,他汀类药物治疗可能是NSCLC患者癌症免疫治疗的联合工具。这些发现应在样本量较大的进一步前瞻性研究中得到验证。
原文来源:
Takada, Kazuki et al. “A propensity score-matched analysis of the impact of statin therapy on the outcomes of patients with non-small-cell lung cancer receiving anti-PD-1 monotherapy: a multicenter retrospective study.” BMC cancer vol. 22,1 503. 6 May. 2022, doi:10.1186/s12885-022-09385-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#单药治疗#
53
#非小细胞#
61
#生存获益#
43
#肺癌患者#
45
是否跟他汀减少动脉粥样硬化斑块或者使用他汀的人被要求禁烟
56
#肿瘤#嗯
51
#非小细胞肺癌患者#
50
很好
63
good
59