Allergy Asthma Immunol Res:过敏性鼻炎患者中外周B细胞子类型分析
2018-05-01 AlexYang MedSci原创
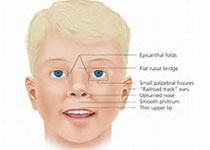
之前证据表明B细胞能够同时促进和抑制过敏性疾病的发展和恶化。然而,在过敏性鼻炎(AR)患者中,B细胞类型的特性情况还没有很好的阐释。最近,有研究人员进行了旨在分析AR患者外周血B细胞类型特性情况的研究。研究包括了57名AR患者和54名健康对照,并且通过流式细胞仪对所有参与者的外周血B细胞类型进行了分析。并且还通过酶联免疫试验测量了血清总lgE和lgE分泌到培养的外周血单核细胞(PBMCs)的浓度情
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#AST#
45
#过敏性#
45
#asthma#
50
#B细胞#
50
#ALL#
33
学习了很有用不错
78
学习了.谢谢分享
69
关注
75