全球首例:中山医院成功完成“CT导引下胰腺射频消融导管治疗胰腺癌”
2016-05-13 介入治疗科 复旦大学附属中山医院微信公众号
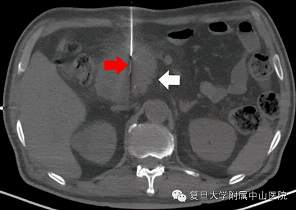
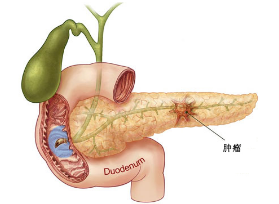
5月10日下午,中山医院介入科专家成功完成全球首例“CT导引下胰腺射频消融导管治疗胰腺癌”。在王小林教授的指导下,陈颐副主任医师带领杨敏捷、高珊珊医师,借助CT精确定位,将直径0.3毫米的Habib射频消融导管在纤细的穿刺针的帮助下,穿刺进入胰腺肿瘤不同部位,进行射频消融治疗。 毫米直径——肿瘤消融治疗器械最“苗条”的导管,仅仅相当于3、4根头发丝的粗细!


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











厉害
113
#射频消融#
24
#消融#
37
#中山医院#
26
好牛啊!
137
值得学习!
116
又一突破。
125
#全球首例#
24