JAMA子刊:肾移植和肝移植孕妈临产:选顺产试产还是直接剖宫产?
2021-10-28 MedSci原创 MedSci原创
与计划性剖宫产术相比,分娩试验能改善新生儿结局,而并不增加母体严重并发症的发病率。
剖宫产(CD)是分娩时最常见的手术操作,占2018年美国产科分娩的31.9%,与CD相关的孕妇并发症包括输血、子宫切除术、产妇出血风险增加、感染、静脉血栓栓塞等,新生儿并发症包括呼吸系统疾病和新生儿重症监护病房(NICU)入院病症等。由于逐步认识到这些风险,临床上开始降低非医学指证的CD。然而,近些年来器官移植患者的CD率越来越高,有必要研究器官移植患者CD的适应症,以确定最安全的产科分娩方式。

这项回顾性队列研究使用了国际移植妊娠注册中心的数据,选取近50年(1968-2019)接受肾脏和肝脏移植的1865名女性来做数据分析研究。数据分析时间为2020年4月30日至2021年4月16日。
参与者的年龄范围为18至48岁,受试者的中位体重指数在正常范围内,接受移植的中位时间间隔超过2年。与计划CD相比,试产(TOL)与肾移植受者的严重孕产妇发病率增加无关。总的来说,459名肾移植受者中有229名(49.9%)和105名肝移植受者中有50名(47.6%)因非药物适应症或重复适应症进行了预定的CDs,尽管有这些适应症的妇女是TOL的候选对象。
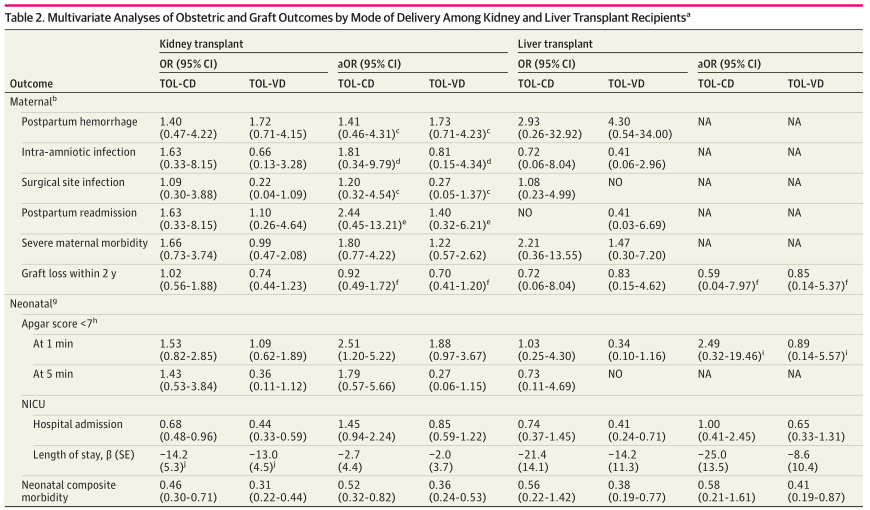
肾和肝移植受者分娩方式对产科和移植结局的多因素分析表
在这项队列研究中,研究者没有发现与分娩试验(TOL)相关的孕产妇发病率增加,尤其是分娩期间高血压疾病恶化导致的急性肾功能衰竭、子痫、肺水肿、中风或心血管并发症风险增加。与计划性剖宫产术相比,分娩试验能改善新生儿结局,而并不增加母体严重并发症的发病率。为了降低器官移植后CD的发病率,可能需要在多个层面进行改革,包括产科和移植团队支持、分娩单位和医院政策改进以及国家和国际支持。在患者的移植中心建立孕前和产前护理可以促进TOL期间更好的跨学科沟通和管理。
参考文献:Yin O, Kallapur A, Coscia L, et al. Mode of Obstetric Delivery in Kidney and Liver Transplant Recipients and Associated Maternal, Neonatal, and Graft Morbidity During 5 Decades of Clinical Practice. JAMA Netw Open. 2021;4(10):e2127378. doi:10.1001/jamanetworkopen.2021.27378
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











有用
42
厉害
50
厉害
60
太厉害了
71