Can J Cardiol:安贞医院学者Meta分析称,TAVI术后出血增加术后30天死亡率
2017-07-19 文韬 中国循环杂志
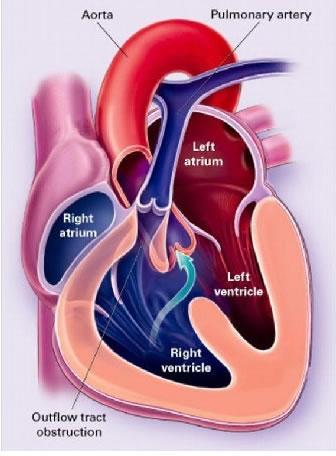
北京安贞医院王家阳等近期一项Meta分析称,对于接受经导管主动脉植入(TAVI)手术的患者,TAVI术后出血的患者术后30天死亡率增加了3倍。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Meta#
38
#安贞医院#
50
#Cardiol#
31
#30天#
34
#MET#
38
很好,不错,以后会多学习
57
学习了涨知识
65
学习了新知识
1
学习了新知识
55