Free Radic Biol Med:血浆中谷蛋白氧还蛋白-1水平可预测心血管疾病患者未来的不良事件
2021-10-09 MedSci原创 MedSci原创
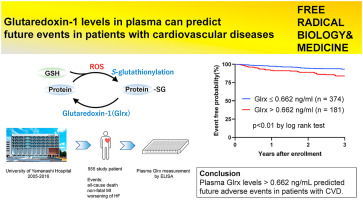
在心血管疾病(CVD)期间增加的活性氧簇通过S-谷胱甘肽化与蛋白质半胱氨酸残基反应形成谷胱甘肽加合物,并通过谷蛋白氧还蛋白-1(Glrx)选择性清除。
在心血管疾病(CVD)期间增加的活性氧簇通过S-谷胱甘肽化与蛋白质半胱氨酸残基反应形成谷胱甘肽加合物,并通过谷蛋白氧还蛋白-1(Glrx)选择性清除。
我们先前的研究表明,S-谷胱甘肽化和Glrx在CVD小鼠模型中发挥重要作用,如心力衰竭和外周动脉疾病模型。但Glrx在CVD中的临床研究较少。虽然Glrx是一种在各种器官中表达的胞质蛋白,但在人血浆中可检测到。研究报道,血浆中的Glrx是一种潜在的疾病标志物,如CVD和慢性肾病及糖尿病,然而,Glrx是否与CVD患者的预后有关仍不清楚。
本研究的目的是阐明血浆中Glrx水平是否与CVD患者未来的事件相关。
采用酶联免疫吸附法检测555例接受心导管检查的CVD患者血浆Glrx水平。所有患者均前瞻性随访≤36个月或直至发生不良事件,包括全因死亡、非致死性心肌梗死和心力衰竭恶化。
在平均33个月的随访期间,发生了54起不良事件。Kaplan-Meier分析显示,与较低水平的Glrx(≤0.622 ng/mL)相比,较高水平的Glrx(> 0.622 ng/mL,由受试者工作特征曲线确定)导致不良事件的概率较高(P < 0.01,对数秩检验)。多因素Cox比例风险分析显示,校正已知危险因素后,Glrx是不良事件的显著预测因子。
总结为以下四点:
1. CVD中ROS增加导致S-谷胱甘肽化,被Glrx清除。
2. Glrx越高,不良事件的概率越高。
3. 血浆中Glrx水平与CVD患者未来的不良事件相关。
3. 校正其他风险因素后,Glrx是不良事件的良好预测因子。
总之,血浆Glrx水平 > 0.662 ng/mL可预测CVD患者未来的不良事件。
原文链接:https://pubmed.ncbi.nlm.nih.gov/34587543/
Glutaredoxin-1 levels in plasma can predict future events in patients with cardiovascular diseases。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言



















#疾病患者#
40
#Bio#
31
#DIC#
27
#Biol#
40
#谷蛋白#
44
#血管疾病#
38
#Med#
36