CAR-T细胞疗法MB-102治疗BPDCN、AML、hrMDS:即将开展多中心I/II期临床试验
2020-10-02 Allan MedSci原创
MB-102是一种CAR-T细胞疗法,通过改造患者T细胞来识别和消除表达CD123的肿瘤。
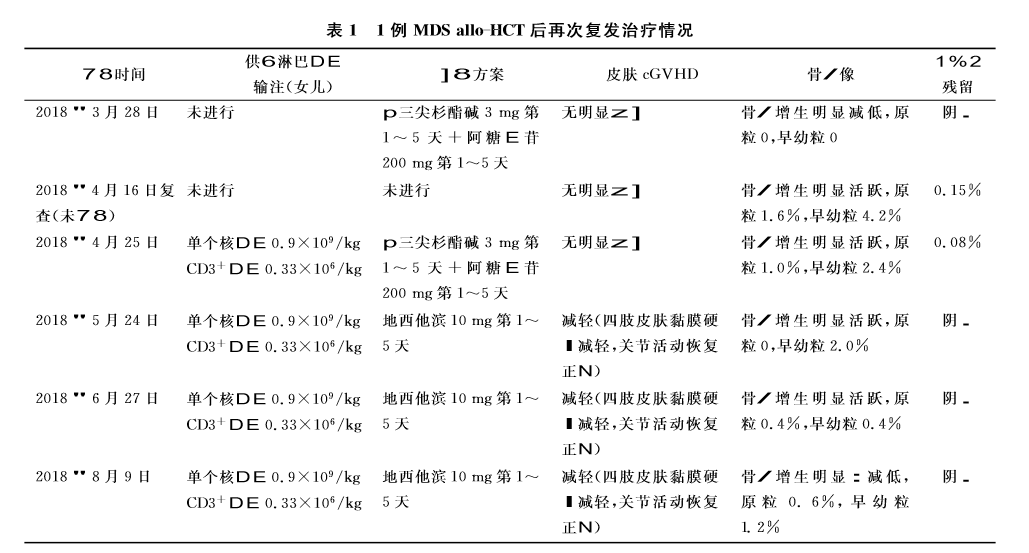
生物公司Mustang近日宣布,首例患者已在多中心I/II期临床试验中接受药物治疗,以评估MB-102(针对CD123的CAR-T细胞疗法)治疗复发难治性母细胞性浆细胞样树突细胞肿瘤(BPDCN)、急性髓细胞性白血病(AML)和高危骨髓增生异常综合征(hrMDS)。研究地点包括希望之城(City of Hope)、丹娜-法伯癌症研究所、杜克大学和MD安德森癌症中心。
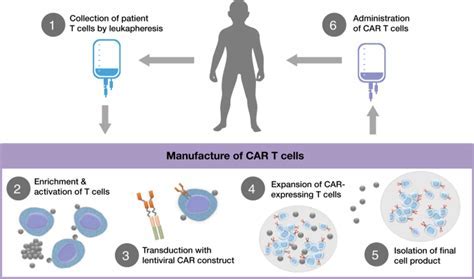
MB-102是一种CAR-T细胞疗法,通过改造患者T细胞来识别和消除表达CD123的肿瘤。CD123在骨髓增生异常综合症患者的骨髓细胞以及包括AML和BPDCN在内的血液系统恶性肿瘤中广泛表达。
试验的第一阶段部分将确定试验的第二阶段部分的MB-102最大耐受剂量。在进行下一个剂量之前,将在每个剂量水平评估安全性。研究的主要终点是所有组输注后第28天的缓解率,次要终点包括反应持续时间、无进展生存期、总体生存期和不良事件的发生率。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#多中心#
39
#CAR-#
49
#I期临床#
36
#I期临床试验#
36
#pDC#
41
#MDS#
45
#II期临床试验#
43
#Car-T细胞疗法#
49
#T细胞疗法#
54
#II期临床#
38