Neuron:帕金森病三十年来新突破!导致运动障碍的罪魁祸首或不是消失的多巴胺
2017-10-22 代丝雨 奇点网
近期发表在《细胞》子刊《神经元》杂志上的一项研究可能要颠覆这一传统认知了。来自韩国科学技术高级研究所(KAIST)和南洋理工大学的科学家发现,增加基底神经节的抑制信号,竟然会让丘脑更加兴奋,从而增加肌肉活动乃至震颤!这也就能解释,为什么很多患者吃了可以增加多巴胺水平的左旋多巴,反倒抖得更加厉害了。
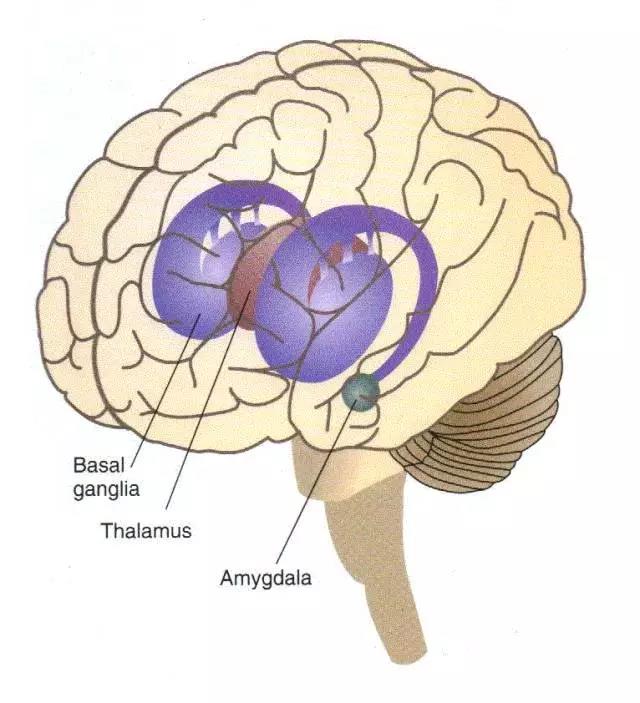
200年前,英国医生James Parkinson描述了一种会不由自主地颤抖的疾病,就是我们现在所说的帕金森病。治疗它的治疗药物有六大类,但是万变不离其宗,它们都是以直接增加脑内多巴胺的水平、或延缓多巴胺的代谢分解为中心来实现治疗目的的。毕竟在大家的认知中,帕金森病的一个主要病理特征就是多巴胺能神经元死亡,多巴胺分泌减少。这导致基底神经节的抑制信号减少,丘脑兴奋的状态就是病因所在。但是!近期发表在《细胞》子刊《神经元》杂志上的一项研究可能要颠覆这一传统认知了。来自韩国科学技术高级研究所(KAIST)和南洋理工大学的科学家发现,增加基底神经节的抑制信号,竟然会让丘脑更加兴奋,从而增加肌肉活动乃至震颤!这也就能解释,为什么很多患者吃了可以增加多巴胺水平的左旋多巴,反倒抖得更加厉害了。棕色为丘脑,紫色为基底神经节基底神经节发出的信号在丘脑汇总,丘脑将运动信号投射到大脑皮层,引起肢体活动大家知道,我们的大脑工作起来是非常复杂的,这个“司令塔”要分成好多个部门。简单来说,“参谋部”基底神经节发出信号,到了“情报中心”丘脑引起神经元的响应,“通信员”大脑皮层得到了动作指令,相应的“执行部队”也就是
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Neuron#
33
#新突破#
28
#运动障碍#
41
学长
64
已学习并已分享
65