ANN ONCOL:Venetoclax联合苯达莫司汀-利妥昔单抗治疗复发/难治性非霍奇金淋巴瘤
2018-09-28 MedSci MedSci原创
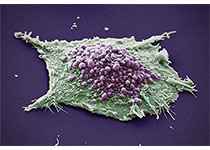
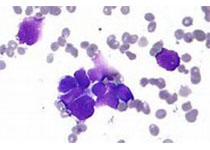
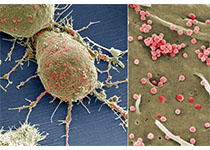
Venetoclax是一种选择性抗细胞凋亡B细胞白血病/淋巴瘤-2蛋白抑制剂,被批准用于治疗慢性淋巴细胞白血病。ANN ONCOL近期发表了一篇文章,报道了venetoclax与苯达莫司汀-利妥昔单抗(BR)联合治疗复发/难治性非霍奇金淋巴瘤(NHL)患者临床试验结果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
29
#NET#
28
#利妥昔#
21
#难治性#
27
#苯达莫司汀-利妥昔单抗#
30
#苯达莫司汀#
38
学习了
52