CGH:入院时血清代谢物和甲状腺素可以预测住院肝硬化患者晚期肝性脑病的发病率
2022-05-09 xuyihan MedSci原创
肝性脑病(HE)又称肝性昏迷,是指严重肝病引起的、以代谢紊乱为基础的中枢神经系统功能失调的综合征,其主要临床表现是意识障碍、行为失常和昏迷。
住院病人发生肝性脑病(HE)后需要一个快速和灵活的策略来保护患者气道,纠正诱发因素,并启动针对HE的治疗。众所周知,晚期肝性脑病(3-4级肝性脑病)需要转移到ICU中进行进一步治疗,如果不及时治疗,会导致吸入性肺炎,并需要插管治疗,此外,晚期肝硬化的发展使移植手术变得复杂。代谢组学已被用于肝硬化的预测,并可能对改善并发症的检测和改善预后有重要作用,代谢组学或对样品中的代谢物进行分析,是一种很有前途的生物标志物发现方法。本项研究的目的是确定入院时的血清代谢物是否能预测未出现晚期肝硬化的患者的发展。
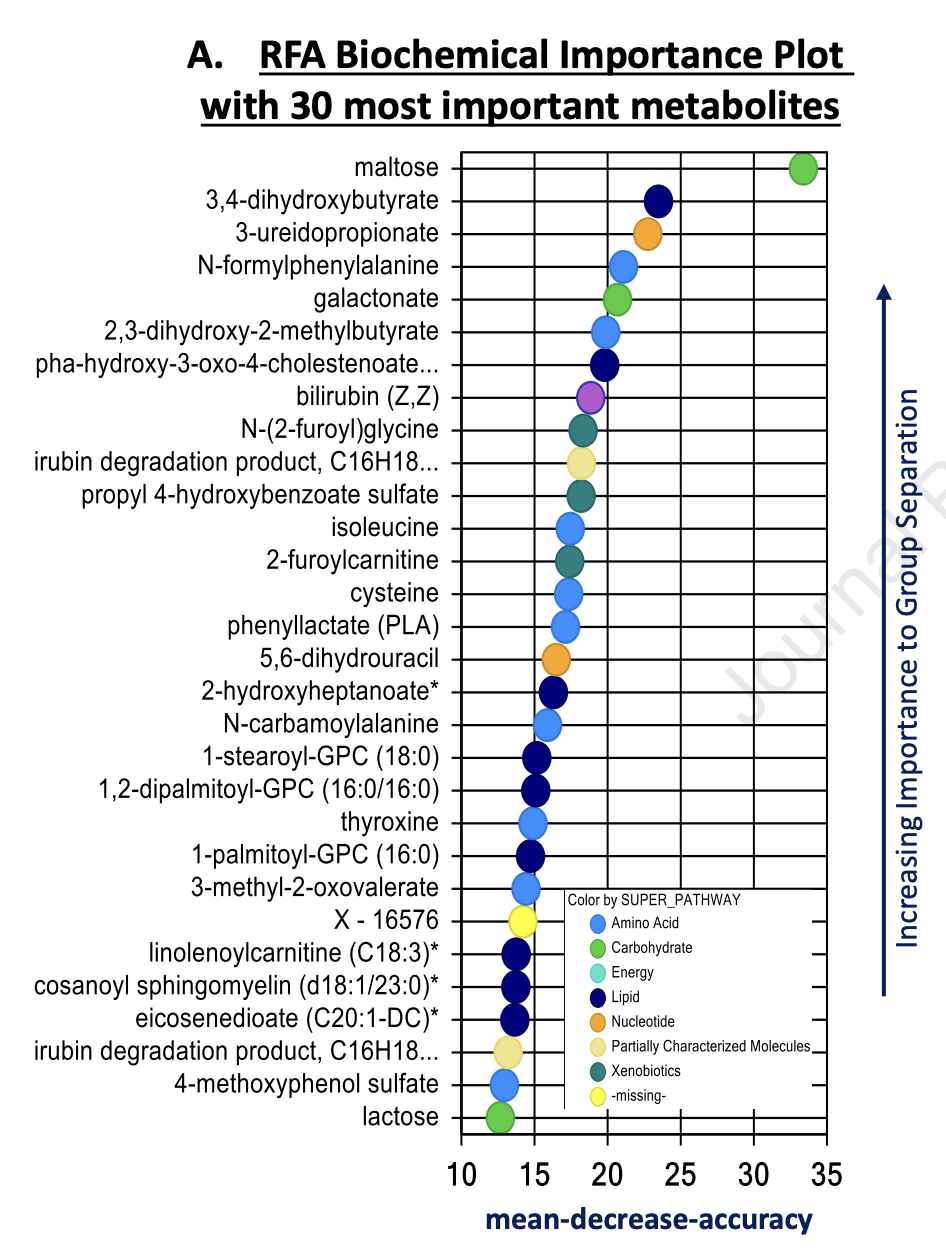
3-4 级肝性脑病(晚期 HE),也称为脑衰竭 (BF),是一种器官衰竭,为了完成本项研究,研究人员在一群没有BF的前瞻性住院肝硬化队列进行了试验,所有患者均接受了入院血清收集和住院随访。血清代谢组学用于预测随机森林分析 (RFA) 。

本项研究纳入的多中心队列中总共包括了602名患者,其中144名患者在入院后3天出现 BF。未经调整的RFA表明,较高的微生物衍生代谢物和较低的异亮氨酸、甲状腺素和溶血磷脂与BF发展相关(AUC=0.87)。BF的预测的四种代谢物是低甲状腺素和麦芽糖以及高 4-羟基苯甲酸甲酯硫酸盐和 3-4 二羟基丁酸。单独的甲状腺素水平也是BF的独立危险因素(p=0.05)。验证队列:前瞻性纳入 81 名患者,其中 11 名发生 BF,侧面验证了本项研究结论。
本项研究结果证实包括甲状腺素在内的入院血清代谢物可以预测晚期 HE 的发展,与临床因素无关。在一个单独的队列中,低当地实验室甲状腺素水平被证实为晚期 HE 发展的预测因子。
原始出处:
Jasmohan S. Bajaj. Et al. Admission Serum Metabolites and Thyroxine Predict Advanced Hepatic Encephalopathy in a Multi-center Inpatient Cirrhosis Cohort. Clinical Gastroenterology and Hepatology.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#代谢物#
55
#脑病#
40
#发病率#
57
#CGH#
63