European Radiology:这一影像学技术,揭示了注意力缺陷/多动症儿童的大脑异常!
2022-06-04 shaosai MedSci原创
铁是儿童大脑发育的关键因素,树突和突触的发育、白质髓鞘化、神经递质(包括多巴胺、去甲肾上腺素、5-羟色胺和GABA)的代谢和分解都需要含铁的酶和铁依赖性蛋白。
 注意力缺陷/多动症(ADHD)是最常见的儿童期神经发育障碍,其特点是与年龄不相称的注意力不集中、多动和冲动,对个人的生活、家庭和社会产生负面影响。尽管临床在多方面进行了深入的研究,但ADHD的发病机制仍不明确。遗传和表观遗传因素、基因和营养的相互作用、环境因素以及压力,都可能导致该疾病的发生。最近的研究表明,多动症可能与缺铁有关,因为在多动症儿童中发现血清铁蛋白水平明显降低。与血清铁不同,脑部铁含量无法直接测量。到目前为止,ADHD患者是否存在脑部铁含量不足以及脑部铁含量与ADHD症状之间的相关性仍不明确。
注意力缺陷/多动症(ADHD)是最常见的儿童期神经发育障碍,其特点是与年龄不相称的注意力不集中、多动和冲动,对个人的生活、家庭和社会产生负面影响。尽管临床在多方面进行了深入的研究,但ADHD的发病机制仍不明确。遗传和表观遗传因素、基因和营养的相互作用、环境因素以及压力,都可能导致该疾病的发生。最近的研究表明,多动症可能与缺铁有关,因为在多动症儿童中发现血清铁蛋白水平明显降低。与血清铁不同,脑部铁含量无法直接测量。到目前为止,ADHD患者是否存在脑部铁含量不足以及脑部铁含量与ADHD症状之间的相关性仍不明确。
铁是儿童大脑发育的关键因素,树突和突触的发育、白质髓鞘化、神经递质(包括多巴胺、去甲肾上腺素、5-羟色胺和GABA)的代谢和分解都需要含铁的酶和铁依赖性蛋白。尽管一些基于ROI的研究发现了基底神经节的铁缺乏,但目前仍没有关于ADHD的全脑铁沉积变化的公开研究。
神经影像技术是一种非侵入性的检查方法,QSM技术可以从梯度回波磁共振相位图像中确定大脑的体磁感应强度分布。近日,发表在European Radiology杂志的一项研究根据增强的ESWAN序列定量测量ADHD儿童的铁沉积,并获取观察到的铁沉积改变的脑区与ADHD疾病严重程度之间的相关性。
本研究纳入了51名6-14岁的临床诊断为多动症的患者和51名年龄和性别相仿的TD儿童。对每个参与者进行3D T1和多回波GRE序列,并使用3.0T MRI获取全脑数据。使用STISuite工具箱计算QSM图。将QSM图像归一到MNI空间后,使用基于体素的分析来比较两组之间的铁含量。使用皮尔逊相关试验评估铁含量和测试分数之间的关联,该测试被用来评估注意力集中程度。
本研究发现,在多动症儿童的几个脑区观察到铁的缺乏,包括双侧纹状体、前小脑回、嗅觉回和右侧舌状回。在进一步的相关分析中,发现左前扣带回与症状的严重程度呈正相关(r = 0.326,p < 0.05)。
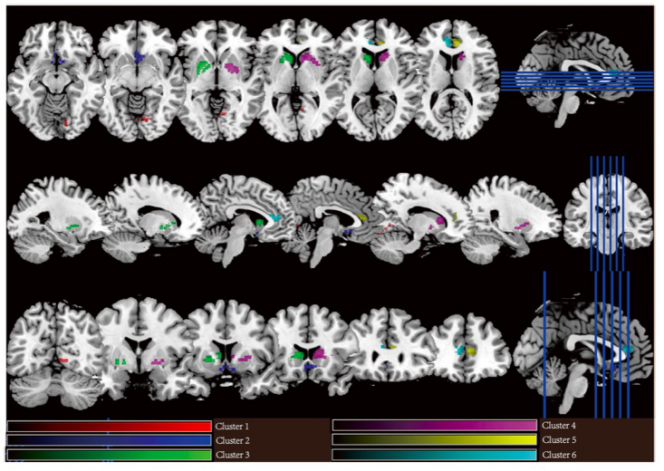
图 聚类显示ADHD和TD儿童在QSM上有明显差异
本研究结果表明,与TD儿童相比,ADHD儿童的几个特定脑区存在铁含量不足,且某些区域的铁含量可能与多动症的症状严重程度有关联。研究结果表明,QSM在ADHD的辅助诊断中具有潜在的功效,且提示这些脑区的铁缺乏可能是ADHD的潜在发病机制。
原文出处:
Yingqian Chen,Shu Su,Yan Dai,et al.Quantitative susceptibility mapping reveals brain iron deficiency in children with attention-deficit/hyperactivity disorder: a whole-brain analysis.DOI:10.1007/s00330-021-08516-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#PE#
33
#脑异常#
47
#多动症#
50
#注意力#
45