CARDIOVASC DIABETOL:在有心血管高风险因素的糖尿病患者中,运动频率与肾脏、心血管转归的关系如何?
2022-02-03 MedSci原创 MedSci原创
体力活动与肾脏结局的关联在有无糖尿病的情况下没有显着差异,但在糖尿病患者中,活动的绝对益处更大。
慢性肾病(CKD)的进展会因合并症和不健康的生活方式(如糖尿病、高血压、不健康的饮食和缺乏运动)而加速。这些相关性往往在糖尿病患者中更强,他们积累了大量心血管(CV)和肾脏事件。
指南建议通过体育锻炼来减少心血管事件。然而体力活动与慢性肾病 (CKD) 进展之间的关联尚不清楚。在这项对先前随机试验项目的事后分析中,研究组对年龄≥55岁的高危患者进行了为期56个月的中位随访,评估了体育活动与肾脏和心血管转归的相关性。研究采用Cox回归分析、重复测量混合模型、方差分析和χ2检验进行分析。共分析31312例患者,其中糖尿病患者19664例,非糖尿病患者11648例。
研究结果显示,体力活动与肾脏结局(肌酐翻倍、终末期肾病(ESRD))和心血管结局(心血管死亡、心肌梗死、中风、心力衰竭住院)呈负相关。与较低的运动水平相比,适度的活动(至少每周2次至每天)与较低的肾脏结局风险和较低的蛋白尿发生率相关。
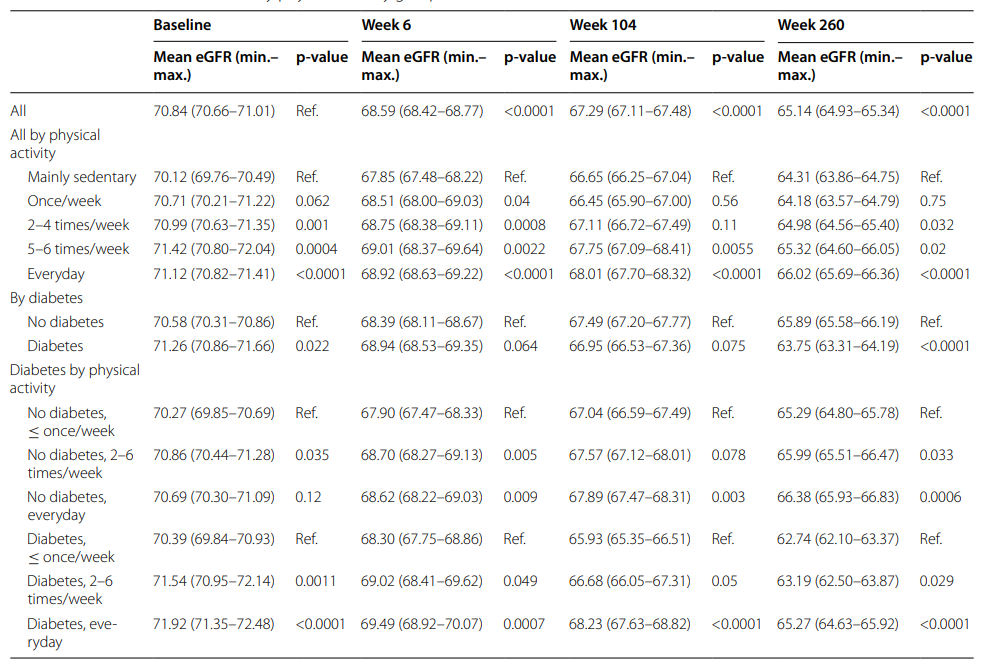
肾脏功能随时间的变化(按体育活动组和糖尿病状况)
对于患有和未患糖尿病的患者,在肾脏结局方面也观察到了类似的结果。体育活动与eGFR下降减少相关,活动与糖尿病状态之间存在中度关联。
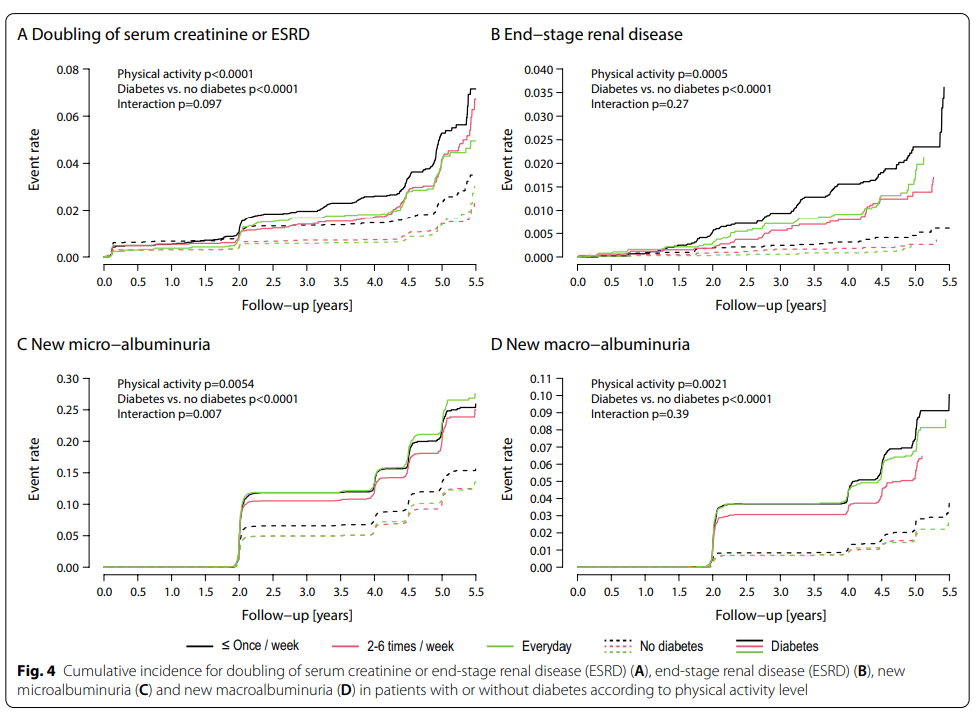
根据运动水平,糖尿病患者或非糖尿病患者血清肌酐或终末期肾病(ESRD) (A)、终末期肾病(B)、微白蛋白尿(C)和大量白蛋白尿(D)增加一倍的累积发病率
总而言之,适度的体育活动与改善肾脏结果相关。体力活动与肾脏结局的关联在有无糖尿病的情况下没有显着差异,但在糖尿病患者中,活动的绝对益处更大。因此,进行高体力活动的糖尿病患者与没有糖尿病但体力活动低的患者之间的风险相似。
参考文献:Böhm, M., Schumacher, H., Werner, C. et al. Association between exercise frequency with renal and cardiovascular outcomes in diabetic and non-diabetic individuals at high cardiovascular risk. Cardiovasc Diabetol 21, 12 (2022). https://doi.org/10.1186/s12933-021-01429-w
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#DIA#
51
#ASC#
34
#BET#
39
#高风险#
45
#糖尿病患者#
37